Yes, frozen shoulder can be a symptom of menopause. Hormonal changes during menopause increase the risk of joint issues, including frozen shoulder. This post will delve into the connection between menopause and the question, “Is frozen shoulder a symptom of menopause?” and discuss effective management strategies.
Key Takeaways
- Frozen shoulder, or adhesive capsulitis, progresses through three phases: freezing, frozen, and thawing, significantly impacting daily activities.
- Hormonal changes during menopause, particularly decreased estrogen levels, heighten the risk of developing frozen shoulder, especially in women aged 40 to 60.
- Effective management of frozen shoulder includes early symptom recognition, various non-surgical treatment options like physical therapy, and potential advanced interventions if necessary.
Understanding Frozen Shoulder
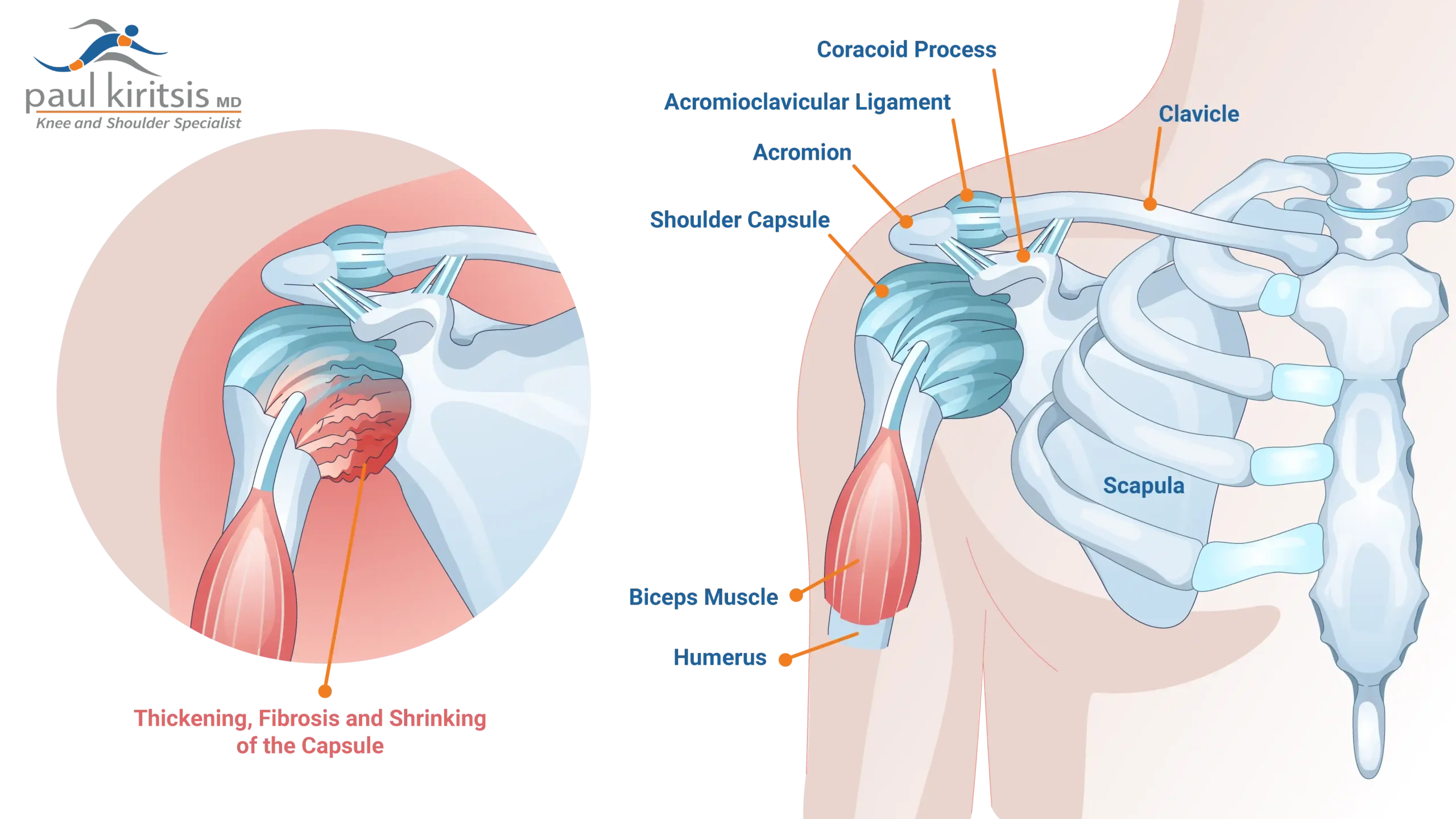
Frozen shoulder, medically termed adhesive capsulitis, is a condition marked by stiffness, swelling, and severe shoulder pain, significantly impacting shoulder motion and daily activities. This condition typically manifests as a limited range of shoulder motion due to the thickening of the shoulder capsule. Initial symptoms often start with severe pain, which gradually becomes a persistent dull ache, greatly affecting daily activities and quality of life.
The progression of frozen shoulder is often categorized into three distinct phases:
- The freezing phase, where pain and stiffness increase.
- The frozen phase, characterized by severe stiffness but reduced pain.
- The thawing phase, where shoulder motion gradually improves.
The condition’s impact on daily life cannot be overstated. Simple tasks like reaching for an object or even letting the affected arm hang naturally can become daunting challenges.
The Connection Between Menopause and Frozen Shoulder
While frozen shoulder can afflict anyone, it is notably more prevalent among women undergoing menopause. More than 50% of people experiencing menopause report joint stiffness, highlighting a significant connection between menopause and frozen shoulder. Furthermore, approximately 70% of individuals with frozen shoulder are women, underscoring the gender-related vulnerability.
The onset of symptoms related to perimenopause typically occurs in women over the age of 40, aligning closely with the ages most affected by frozen shoulder, which is between 40 and 60 years. Recognizing this connection offers a clearer path for managing and treating frozen shoulder in menopausal women.
Hormonal changes during menopause
Menopausal hormonal fluctuations significantly affect the body, especially connective tissues. Estrogen, a hormone that plays a crucial role in promoting connective tissue integrity and elasticity, declines significantly during menopause. Decreased estrogen levels lead to shoulder joint stiffness and reduced flexibility.
The changes in estrogen levels can also alter collagen production and turnover, further affecting joint health. With the decline in estrogen, there is a relative increase in inflammation, contributing to joint issues like frozen shoulder.
Symptoms of Frozen Shoulder During Menopause
Frozen shoulder during menopause is characterized by the presence of fibrous tissue that restricts shoulder movement, leading to significant discomfort. High levels of stress and disturbed sleep patterns often accompany perimenopausal women, which can exacerbate frozen shoulder symptoms. Recognizing these symptoms early can lead to more effective management and treatment.
Recognizing early signs
The initial signs of frozen shoulder typically include persistent shoulder pain and a noticeable decrease in the mobility of the affected shoulder. These early symptoms often present as a dull ache in the shoulder area, making routine tasks more challenging. Early recognition of these signs facilitates effective management and treatment.
Progression of symptoms
As frozen shoulder progresses, individuals often notice a gradual increase in shoulder stiffness and pain during the freezing phase, which impacts their daily activities. During this phase, the shoulder becomes increasingly difficult to move, complicating routine tasks. The frozen stage, although seeing an alleviation of pain, is marked by persistent stiffness that continues to hinder daily activities.
In the thawing stage, shoulder mobility gradually returns, and individuals experience an improvement in their daily function.
Diagnosing Frozen Shoulder in Menopausal Women
Diagnosing frozen shoulder in menopausal women involves a combination of clinical examination and imaging techniques.
Reviewing medical history is important for diagnosing frozen shoulder in menopausal women, helping to identify any past shoulder injuries or conditions. During the clinical evaluation, an orthopedic shoulder surgeon assesses both active and passive ranges of motion to determine the extent of mobility issues in the shoulder. This assessment clarifies the condition’s severity and guides appropriate treatment planning.
Imaging techniques such as MRI are not needed in diagnosing frozen shoulder. This diagnosis is primarily achieved through a detail physical exam.
Treatment Options for Menopause-Related Frozen Shoulder
There are several effective treatment options available for managing frozen shoulder during menopause. These treatments range from non-surgical interventions to advanced surgical procedures.
Knowing these options aids in making informed decisions about managing the condition.
Non-surgical treatments
Non-surgical treatments for frozen shoulder include physical therapy, medications, and lifestyle modifications. Over-the-counter anti-inflammatory drugs like ibuprofen can help alleviate swelling and discomfort associated with frozen shoulder. Performing shoulder-specific stretching and strengthening exercises enhances flexibility and muscle support.
Physical therapy can play an important role to regain shoulder movement. Gentle stretching and physical therapy significantly alleviate frozen shoulder symptoms by enhancing movement and strength. A home exercise program is imperative in the treatment regiment for a frozen shoulder and moist heat, including hot showers are often helpful.
Advanced interventions
When conservative treatments fail, advanced interventions such as shoulder manipulation under anesthesia and minimally invasive arthroscopy may be necessary to restore shoulder mobility. These surgical options aim to free the joint from adhesions and improve the range of motion, often performed by a specialist shoulder surgeon.
Advanced interventions can significantly enhance quality of life and restore functionality for those struggling with persistent frozen shoulder symptoms.
Preventative Measures and Lifestyle Adjustments
Preventative measures and lifestyle adjustments can play a significant role in reducing the risk of developing frozen shoulder during menopause. These practices help maintain shoulder health and flexibility.
Promoting joint health
Maintaining proper posture throughout daily activities helps prevent imbalances that may lead to shoulder issues. Incorporating gentle stretching and mobility exercises into daily routines can aid in managing symptoms and improving function.
Regular physical activity, such as swimming or yoga, can promote shoulder motion and enhance overall joint health.
Managing hormonal balance
Hormone replacement therapy can manage menopause-related hormonal changes and may benefit shoulder health. Hormonal therapy may alleviate frozen shoulder discomfort by stabilizing menopausal hormonal fluctuations.
Balancing hormones can indirectly support shoulder health and reduce frozen shoulder risk.
Coping Strategies for Daily Life
Coping with daily activities while managing frozen shoulder can be challenging. Effective strategies can alleviate discomfort and improve quality of life.
Sleep positions
Sleeping on your back minimizes pressure on the joint and allows better rest for frozen shoulder. If back sleeping is uncomfortable, lying on the unaffected side with supportive pillows can help keep the affected shoulder stable.
A supportive pillow can maintain neck and shoulder alignment, reducing sleep discomfort.
Modifying activities
Adjusting daily routines, like avoiding overhead lifting or heavy reaching, accommodates limited shoulder movement. Adaptive tools and adjusted work surface heights can minimize shoulder strain.
These modifications can help manage shoulder pain and conserve energy, making everyday tasks more manageable.
Summary
Understanding the connection between menopause and frozen shoulder is crucial for effective management and treatment. By recognizing the symptoms early, seeking timely medical advice, and incorporating appropriate treatments and lifestyle adjustments, women can significantly alleviate the discomfort associated with frozen shoulder during menopause.
Frequently Asked Questions
What is frozen shoulder, and what are its symptoms?
Frozen shoulder, or adhesive capsulitis, results in significant stiffness and pain in the shoulder joint, which can severely limit movement. Symptoms include restricted range of motion, intense pain, and a constant dull ache that affects daily activities.
How is menopause related to frozen shoulder?
Menopause is linked to frozen shoulder due to decreased estrogen levels, which can increase inflammation and joint stiffness, making women more prone to this condition. Therefore, hormonal changes during menopause can heighten the risk of developing frozen shoulder.
What are the early signs of frozen shoulder during menopause?
The early signs of frozen shoulder during menopause include persistent shoulder pain, decreased shoulder mobility, and a dull ache in the shoulder area. Addressing these symptoms promptly can facilitate better management and treatment.
What are the non-surgical treatment options for frozen shoulder?
Non-surgical treatment options for frozen shoulder include physical therapy, stretching and strengthening exercises, over-the-counter anti-inflammatory medications such as ibuprofen, and injections. These approaches effectively alleviate symptoms and enhance shoulder mobility.
How can I prevent frozen shoulder during menopause?
To prevent frozen shoulder during menopause, focus on maintaining proper posture, engage in gentle stretching and mobility exercises, and consider hormone replacement therapy to manage hormonal changes. Implementing these strategies can significantly reduce your risk.





