Reverse Shoulder Replacement
Office Location
Discover Dr. Kiritsis' Precision Shoulder Replacement
Dr. Kiritsis' Specialties
Call Dr. Kiritsis to Schedule an Appointment
Reverse Shoulder Replacement
Disorders of the Shoulder | Precision Shoulder Replacement | Reverse Shoulder Replacement
Introduction
Shoulder joint replacement surgery (also called shoulder arthroplasty) can effectively ease pain from shoulder arthritis.
Most people experience improved shoulder function after this surgery. But, certain patients are not candidates for joint replacement of the shoulder because they lack the muscle function necessary to stabilize the joint.
A different type of shoulder replacement, called reverse shoulder replacement, may be available for many of these patients and provide pain relief as well as a stable functioning shoulder.
This guide will help you understand
- How the shoulder works
- What parts of the shoulder are replaced in reverse shoulder replacement
- How to reverse shoulder replacement differs from shoulder replacement
- What to expect after reverse shoulder replacement surgery

What parts of the shoulder are involved?
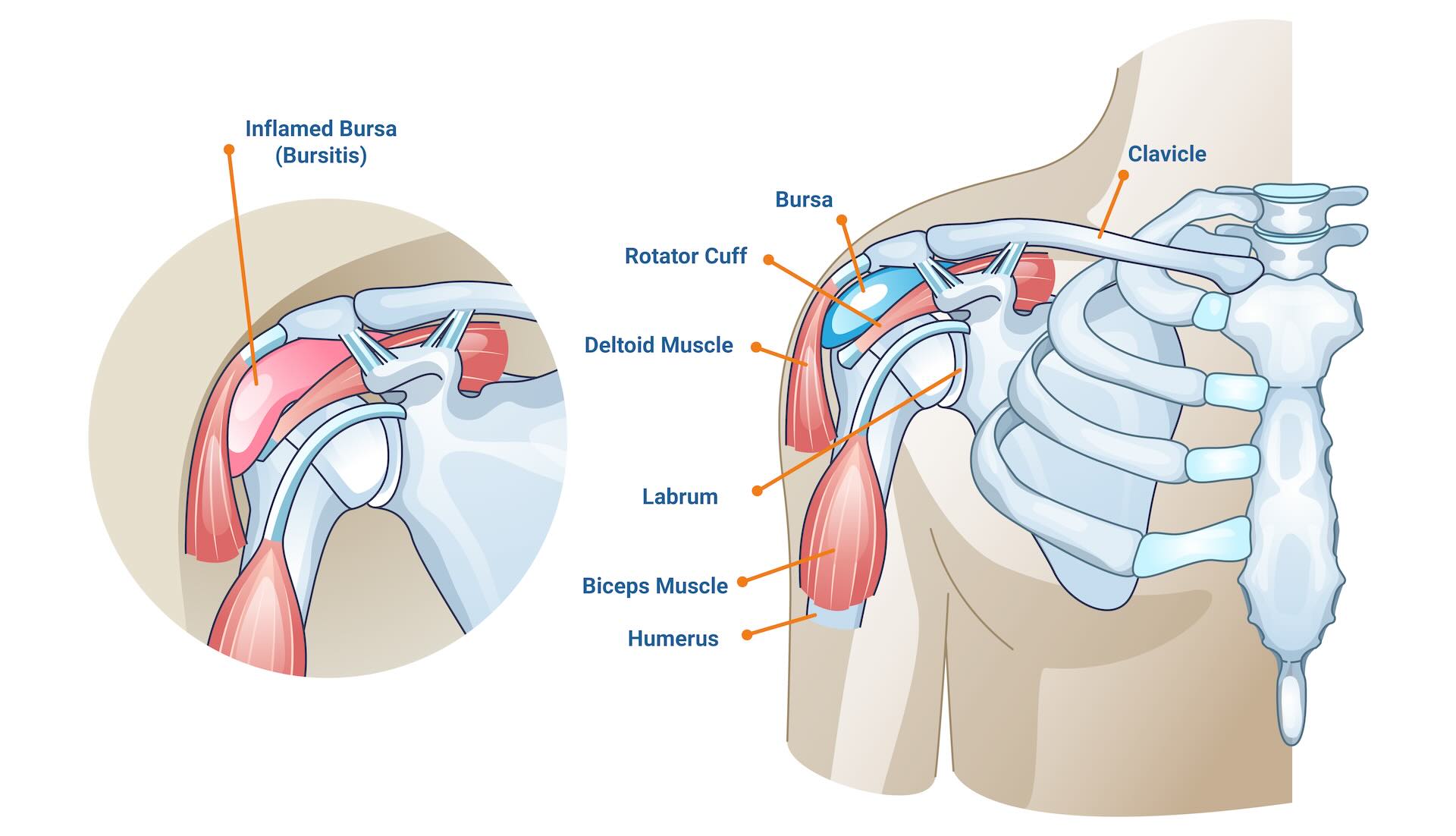
The shoulder is made up of three bones: the scapula (shoulder blade), the humerus (upper arm bone), and the clavicle (collarbone).
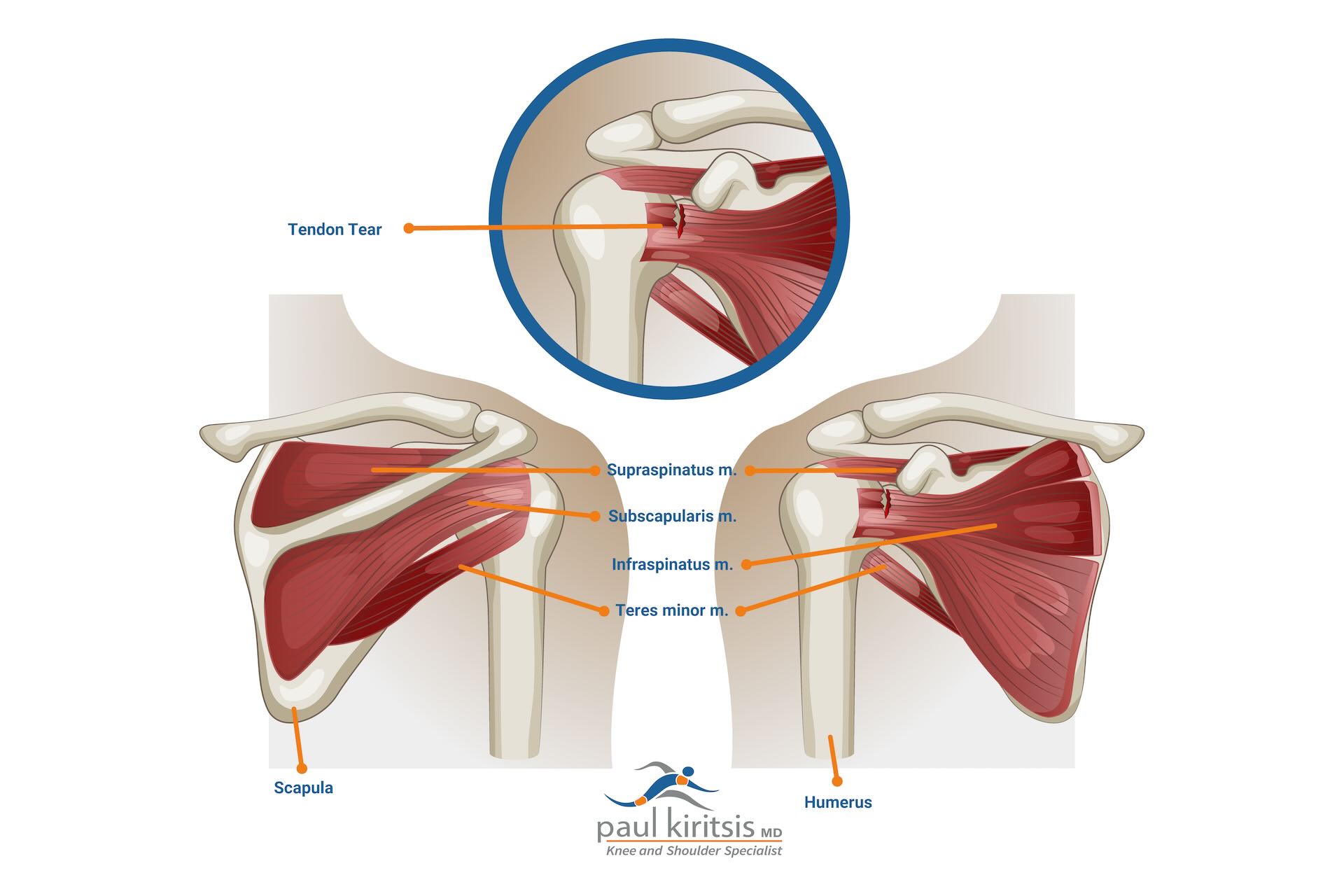
The rotator cuff connects the humerus to the scapula. The rotator cuff is formed by the tendons of four muscles: the supraspinatus, infraspinatus, teres minor, and subscapularis.
Muscles move bones by pulling on the tendons. The rotator cuff helps raise and rotate the arm. As the arm is raised, the rotator cuff also keeps the humerus tightly in the socket.
A part of the scapula, called the glenoid, makes up the socket of the shoulder. The glenoid is very shallow and flat.
The part of the scapula that connects to the shoulder is called the acromion. A bursa is located between the acromion and the rotator cuff tendons. A bursa is a lubricated sac of tissue that cuts down on the friction between two moving parts.
Bursae are located all over the body where tissues must rub against each other. In this case, the bursa protects the acromion and the rotator cuff from grinding against each other.
The humeral head of the shoulder is the ball portion of the joint. The humeral head has several blood vessels, which enter at the base of the articular cartilage. Articular cartilage is the smooth, white material that covers the ends of bones in most joints.
Articular cartilage provides a slick, rubbery surface that allows the bones to glide over each other as they move. Cartilage also functions as sort of a shock absorber.
The shoulder joint is surrounded by a watertight sac called the joint capsule. The joint capsule holds fluids that lubricate the joint. The walls of the joint capsule are made up of ligaments. Ligaments are connective tissues that attach bones to bones.
The joint capsule has a considerable amount of slack, loose tissue so that the shoulder is unrestricted as it moves through its large range of motion.
Rationale
What conditions lead to reverse shoulder joint replacement?
The most common reason for undergoing shoulder replacement surgery is osteoarthritis.
Osteoarthritis is caused by the degeneration of the joint over time, through wear and tear. Osteoarthritis can occur without any injury to the shoulder, but that is uncommon. Because the shoulder is not a weight-bearing joint, it does not suffer as much wear and tear as other joints. Osteoarthritis is more common in the hip and knee.
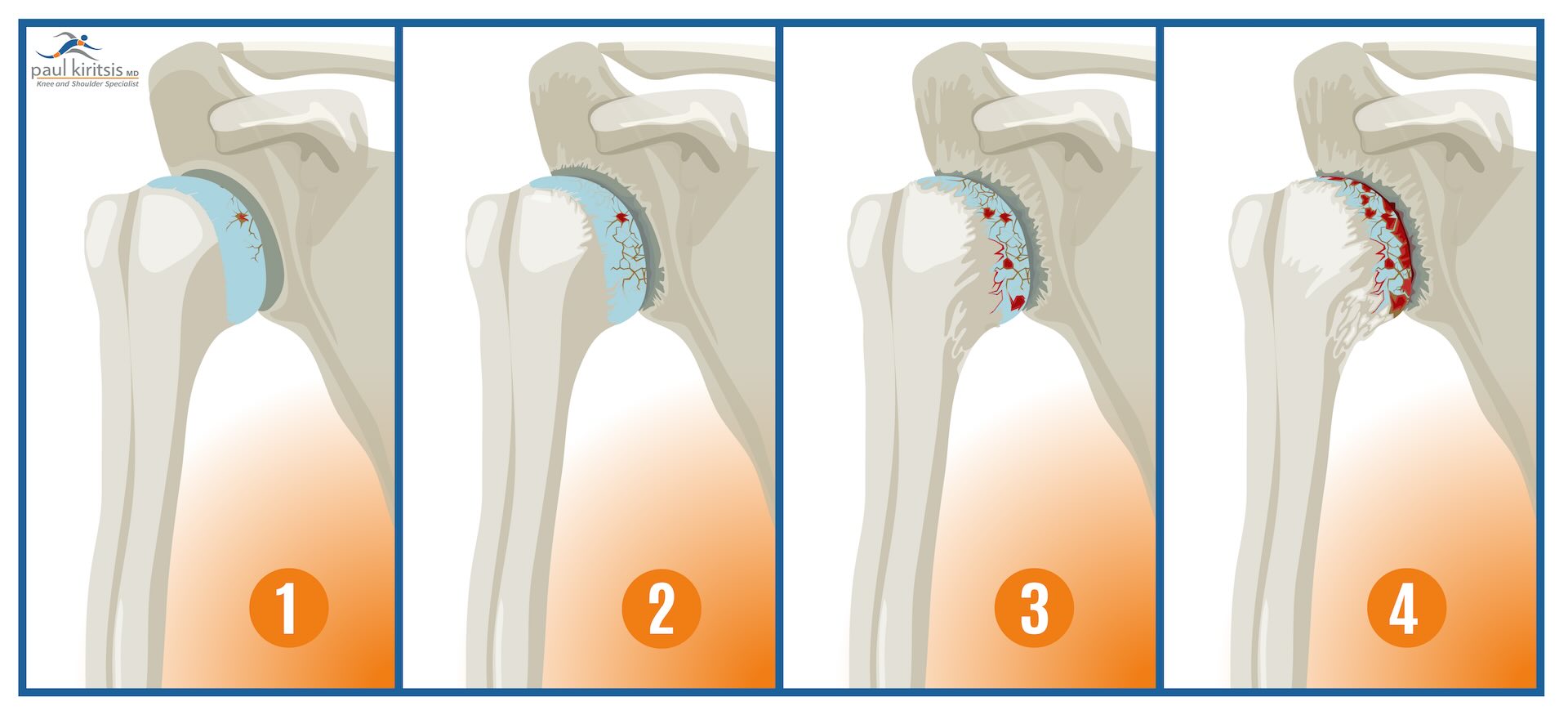
Rotator cuff problems are a common condition in the shoulder, especially as we grow older. Degeneration or wear and tear of the rotator cuff tendons occurs as we age. Over time this can lead to the weakening of the tendons and may result in a rotator cuff tear.
Surgery to repair a rotator cuff tear is fairly common in people who are middle-aged and older. Most rotator cuff repairs are successful, but in a portion of patients, the tendon has become so degenerated that the tendon can simply not be repaired.
Small, medium, and many large tears can be repaired through arthroscopic techniques. Unfortunately, many large tears that are untreated for a long time may retract and become unfixable. A shoulder joint without an intact rotator cuff may still function relatively well.
However, patients with massive rotator cuff tears may not be able to lift their arms without significant pain and weakness. When the arm cannot be lifted, this is called a pseudoparalytic shoulder. The shoulder needs a functioning rotator cuff to remain stable as well as to create a joint capsule to hold the joint fluid that lubricates the joint.
Over time, a shoulder without an intact rotator cuff becomes arthritic – the shoulder joint wears out due to abnormal motion, instability, and lack of lubrication from the joint fluid. This type of wear and tear arthritis in the shoulder is called (rotator) cuff tear arthropathy.
Cuff tear arthropathy is difficult to treat. The shoulder is weak and painful. Patients may not be able to raise the arm above shoulder level.
Patients with this type of arthritis would seem to be good candidates for a shoulder replacement, but replacing the shoulder in the typical fashion has not been successful.
The normal artificial shoulder was designed to copy our real shoulder. The glenoid component (the socket) was designed to replace our normal shoulder socket with a thin, shallow plastic cup.
The humeral head component was designed to replace the ball of the humerus with a metal ball that sits on top of the glenoid. This situation has been compared to placing a ball on a shallow saucer. Without something to hold it in place, the metal ball simply slides around on the saucer.
In the shoulder, that something is the rotator cuff and the muscles that attach to the tendons. Without a rotator cuff to hold the metal ball centered in the plastic socket, the metal quickly wore out the plastic socket and the joint became painful once again.
The answer to this dilemma was to rethink the mechanics of the shoulder joint and design an artificial shoulder that worked differently than the real shoulder joint.
The solution was to reverse the socket and the ball, placing the ball portion of the shoulder where the socket use to be and the socket where the ball or humeral head used to be.
This new design led to a much more stable shoulder joint that could function without a rotator cuff. The artificial joint itself provided more stability by creating a deeper socket that prevented the ball from sliding up and down as the shoulder was raised.
The large deltoid muscle that covers the shoulder could be used to lift the arm, providing a better function for the shoulder. The final result is a shoulder that functions better is less painful and can last for years without loosening.
Other reasons to consider a reverse shoulder replacement include failed rotator cuff surgery leading to a pseudoparalytic shoulder even without arthritis.
A pseudoparalytic shoulder refers to a situation where you can not raise the shoulder. Pseudo means false and paralysis usually means that the nerves that control the muscle no longer control the muscles.
A pseudoparalytic shoulder appears paralyzed, but the reason that you cannot raise the shoulder is that the rotator cuff tendons that attach the muscles (that raise the shoulder) to the humerus bone are torn. The power of the muscles cannot be transmitted to the humerus to raise the shoulder.
Older patients with very severe fractures of the head of the humerus appear to do very well with reverse shoulder replacements as opposed to a standard partial shoulder replacement.
Patients who have had previous shoulder replacements that have failed or become loose will also require a reverse shoulder replacement to fix the loose or painful prosthesis.
Dr. Kiritsis will want you to try nonsurgical measures to control your pain and improve your shoulder movement, including medications and physical or occupational therapy.
Like any arthritic condition, cuff tear arthropathy of the shoulder may respond to anti-inflammatory medications such as Alleve or ibuprofen.
Acetaminophen (Tylenol) may also be prescribed to ease the pain. Some of the newer medications such as glucosamine and chondroitin sulfate may be helpful. They seem to be effective in helping reduce the pain of arthritis in all joints.
Physical or occupational therapy may be suggested to help you regain as much of the motion and strength in your shoulder as possible before you undergo surgery.
In many cases, however, therapy may not be indicated for severe shoulder arthritis since it may aggravate the pain. This is a matter to be discussed with Dr. Kiritsis.
An injection of cortisone into the shoulder joint may give temporary relief. Cortisone is a powerful anti-inflammatory medication that can ease inflammation and reduce pain, possibly for several months.
Most surgeons only allow two or three cortisone shots into any joint. If the shots don’t provide you with lasting relief, Dr. Kiritsis may suggest surgery.
Preparing for Surgery
What do I need to do to get ready for surgery?
When cuff tear arthropathy of the shoulder requires replacement of the painful shoulder with an artificial shoulder joint, a reverse shoulder replacement may be recommended.
You and Dr. Kiritsis should make the decision to proceed with surgery together. You need to understand as much about the procedure as possible. If you have concerns or questions, you should discuss them with Dr. Kiritsis.
Once you decide on surgery, you need to take several steps. Dr. Kiritsis will suggest a complete physical examination by your regular doctor. This exam helps ensure that you are in the best possible condition to undergo the operation.
Special x-rays will be needed. Plain x-rays of the shoulder will allow Dr. Kiritsis to evaluate the severity of arthritis and the status of the rotator cuff.
A CT scan is typically required before any kind of shoulder replacement to determine the degree of damage to the bones (glenoid and humeral head) for surgical planning.
You may also need to spend time with the physical or occupational therapist who will be managing your rehabilitation after surgery. This allows you to get a head start on your recovery. One purpose of this pre-operative visit is to record a baseline of information.
Your therapist will check your current pain levels, your ability to do your activities, and the movement and strength of each shoulder.
A second purpose of the pre-operative visit is to prepare you for surgery. You’ll begin learning some of the exercises you will use during your recovery.
Your therapist can help you anticipate any special needs or problems you might have at home, once you’re released from the hospital.
On the day of your surgery, you will probably be admitted to the hospital early in the morning. You shouldn’t eat or drink anything after midnight the night before. Come prepared to stay in the hospital for one night.
The Reverse Artificial Shoulder
The reverse shoulder prosthesis (artificial joint) is made up of two parts. The humeral component replaces the humeral head or the ball of the joint.
The glenoid component replaces the socket of the shoulder, which is actually part of the scapula.
In the normal artificial shoulder prosthesis, the glenoid prosthesis is a shallow socket made of plastic and the humeral component is a metal stem attached to a metal ball that nearly matches the anatomy of the normal shoulder.
In the reverse shoulder replacement, the ball and the socket are reversed.
The humeral component is a combination of a metal stem that fits into the marrow cavity of the upper humerus and, on top of the metal stem, a plastic socket.
This plastic socket fits onto the humeral component to create a ball and socket-type bearing. The glenoid component is usually made of two parts.
A metal tray (base plate) attaches directly to the bone. The glenoid base plate is inserted into a small peg hole drilled into the bone and is secured with special screws through the base plate into the bone.
Attached to that metal tray, a metal ball is attached that will fit into the plastic socket attached to the humeral component.
The plastic is very tough and very slick, much like the articular cartilage it is replacing.
In fact, you can ice skate on a sheet of this plastic without causing it much damage.
The Operation
The reverse shoulder replacement surgery is performed almost identically to the normal shoulder replacement – except different artificial parts are inserted.
You will most likely need general anesthesia for shoulder replacement surgery. General anesthesia puts you to sleep. You will have a regional nerve block which will significantly reduce your postoperative pain.
Shoulder replacement surgery is done through an incision on the front of your shoulder. This is called an anterior (deltopectoral) approach.
Dr. Kiritsis enters the shoulder joint itself by cutting into the joint capsule. This allows him to see the joint. In more advanced cases of cuff tear arthropathy, and in patients with previous surgery, there may be no capsule and rotator cuff remaining.
At this point, Dr. Kiritsis can prepare the bone for attaching the replacement parts. The ball portion of the humeral head is removed with a bone saw. The hollow inside of the upper humerus is prepared using a broach. This lets Dr. Kiritsis mold the space to anchor the metal stem of the humeral component inside the bone.
The glenoid will be replaced with a ball of metal. The arthritic glenoid surface is prepared by grinding away any remaining cartilage and flattening the surface.
This is done with an instrument called a reamer. Dr. Kiritsis usually uses the reamer to drill holes into the bone of the scapula and flatten the deformed glenoid surface so the base plate rests on a smooth, flat surface. This is where the stem of the glenoid component is anchored.
Finally, the humeral component and the glenoid component are inserted.
Once the joint is anchored, Dr. Kiritsis tests for proper fit and begins to close the wound. The muscles are then returned to their correct positions, and the skin is also sutured.
Your incision will be covered with a bandage, and your arm will be placed in a sling. You will then be awakened and taken to the recovery room.
Potential Complications
What might go wrong?
As with all major surgical procedures, complications can occur. This document doesn’t provide a complete list of the possible complications, but it does highlight some of the most common problems. Some of the most common complications following artificial shoulder replacement are
- anesthesia
- infection
- loosening
- dislocation
- nerve or blood vessel injury
Anesthesia
Most surgical procedures require that some type of anesthesia be done before surgery. A very small number of patients have problems with anesthesia.
These problems can be reactions to the drugs used, problems related to other medical complications, and problems due to the anesthesia. Be sure to discuss the risks and your concerns with your anesthesiologist.
Infection
Infection following joint replacement surgery can be very serious. The chances of developing an infection following artificial joint replacement, however, are low (less than one percent).
Sometimes infections show up very early. Other times infections may not show up for months, or even years, after the operation.
Infection can also spread into the artificial joint from other infected areas. Once an infection lodges in your joint, it is almost impossible for your immune system to clear it. Multiple surgeries are typically required to treat an infected joint.
Loosening
The major reason that artificial joints eventually fail is that they loosen where the metal or cement meets the bone. A loose joint prosthesis causes pain. Once the pain becomes unbearable, another operation will probably be needed to fix the artificial joint.
There have been great advances in extending the life of artificial joints. However, most will eventually loosen and require another surgery. In the case of artificial knees, you can expect at least 15 years, but artificial shoulder joints may loosen sooner.
Dislocation
Just like your real shoulder, an artificial shoulder can dislocate. A shoulder dislocation occurs when the ball comes out of the socket. There is a greater risk of dislocation right after surgery before the tissues have healed around the new joint.
But there is always a slightly increased risk of dislocation with an artificial joint. Your therapist will teach you how to avoid activities and positions that tend to cause a shoulder dislocation. A shoulder that dislocates more than once may need another operation to make it more stable.
Nerve or Blood Vessel Injury
All of the large nerves and blood vessels to the arm and hand travel through the armpit. (This area is called the axilla.) Because shoulder replacement surgery takes place so close to the axilla, it is possible that the nerves or blood vessels may be injured during surgery.
The resulting problems may be temporary if the injury was caused by stretching to hold the nerves out of the way. The nerves and blood vessels rarely suffer any kind of permanent injury after shoulder replacement surgery, but this type of injury can happen.
After Surgery
What happens after surgery?
After surgery, you’ll be transported to the recovery room. You will have a dressing wrapped over your shoulder that will stay in place until your office follow-up. An intravenous line (IV) will be placed in your arm to give you the needed antibiotics and medication.
Rehabilitation
What will my recovery be like?
A physical or occupational therapist will see you the day after surgery to begin your rehabilitation program. Therapy treatments will gradually improve the movement in your shoulder. Your therapist will go over your exercises and make sure you are safe getting in and out of bed and moving about in your room.
When you go home, you will typically attend outpatient therapy. Treatments will be done to help improve your range of motion and strength.
The first few outpatient treatments will focus on controlling pain and swelling. Ice and electrical stimulation treatments may help. Your therapist may also use massage and other types of hands-on treatments to ease muscle spasms and pain. Continue to use your shoulder sling for four weeks.
As the rehabilitation program evolves, more challenging exercises are chosen to safely advance the shoulder’s strength and function.
Finally, a select group of exercises can be used to simulate day-to-day activities, like grooming your hair or getting dressed. Specific exercises may also be chosen to simulate work or hobby demands.
When your shoulder range of motion and strength have improved enough, you’ll be able to gradually get back to normal activities. Ideally, you’ll be able to do almost everything you did before. However, you may need to avoid heavy or repeated shoulder actions.
You may be involved in a progressive rehabilitation program for two to four months after surgery to ensure the best results from your artificial joint. In the first six weeks after surgery, you should expect to see your therapist two to three times a week. At that time, if everything is still going as planned, you may be able to advance to a home program. Then you will only check in with your therapist every few weeks.


Paul Kiritsis, MD
Dr. Kiritsis, a Richmond native, is one of a select number of Orthopedic Surgeons in the Richmond area to hold a second subspecialty board certification in Sports Medicine.
