Meniscal Surgery
Office Location
Dr. Kiritsis' Specialties
Call Dr. Kiritsis to Schedule an Appointment
Knee Meniscal Surgery
Disorders of the Knee | Orthopedic Surgery | Meniscus
The meniscus is very important to the long-term health of the knee. In the past, surgeons would simply take out part or all of an injured meniscus. But today’s surgeons know that removing the meniscus can lead to early knee arthritis.
Whenever possible, they try to repair the tear. If the damaged area must be removed, care is taken during surgery to protect the surrounding healthy tissue.
This guide will help you understand
- what parts of the knee are treated during meniscal surgery
- what operations are used to treat a damaged meniscus
- what to expect before and after meniscal surgery
Related Document: A Patient’s Guide to Meniscal Injuries
Anatomy
What parts of the knee are involved?
There is one meniscus on each side of the knee joint. The C-shaped medial meniscus is on the inside part of the knee, closest to your other knee. (Medial means closer to the middle of the body.) The U-shaped lateral meniscus is on the outer half of the knee joint. (Lateral means further out from the center of the body.)
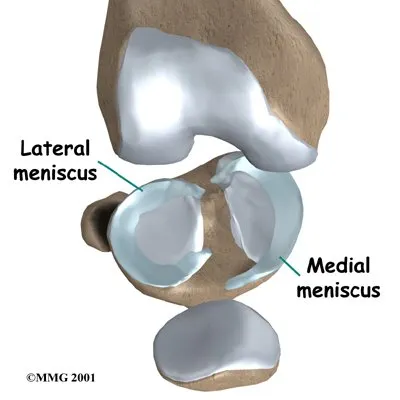
The menisci (plural for meniscus) protect the articular cartilage on the surfaces of the thighbone (femur) and the shinbone (tibia). Articular cartilage is the smooth, slippery material that covers the ends of the bones that make up the knee joint. The articular cartilage allows the joint surfaces to slide against one another without damage to either surface.
Most of the meniscus is avascular, meaning no blood vessels go to it. Only its outer rim gets a small supply of blood. Doctors call this area the red zone. The ends of a few vessels in the red zone may actually travel inward to the middle section, the red-white zone.
The inner portion of the meniscus, closest to the center of the knee, is called the white zone. It has no blood vessels at all. Although a tear in the outer rim has a good chance of healing, damage further toward the center of the meniscus will not heal on its own.
Related Document: A Patient’s Guide to Knee Anatomy
Rationale
What does Dr. Kiritsis hope to accomplish?
The meniscus is a pad of cartilage that acts like a shock absorber to protect the knee. The meniscus is also vital for knee stability. When the meniscus is damaged or is surgically removed, the knee joint can become loose, or unstable. Without the protection and stability of a healthy meniscus, the surfaces of the knee can suffer wear and tear, leading to a condition called osteoarthritis.
Related Document: A Patient’s Guide to Knee Osteoarthritis
Most tears of the meniscus do not heal on their own. A small tear in the outer rim (the red zone) has a good chance of healing.
However, tears in the inner part of the meniscus often require surgery. When tears in this area are causing symptoms, they tend to get bigger. This puts the articular cartilage on the surfaces of the knee joint at risk of injury.
Dr. Kiritsis’ primary goal is to save the meniscus. If an injured part must be removed, only the smallest amount of the meniscus is taken out. Preserving the nearby areas of the meniscus is vital for keeping the knee healthy. If a tear can possibly be repaired, Dr. Kiritsis will recommend a meniscal repair.
A torn meniscus may cause symptoms of pain and swelling and sometimes catching and locking. The goal of surgery is to take these symptoms away. When the knee locks and you have to tug on it to get it moving, a small flap from a meniscal tear may have developed.
The flap may be getting caught in the knee joint as you bend it. Or a small piece of the meniscus could actually be floating around inside the joint. This fragment, called a loose body, can get lodged between the moving parts of the knee, causing the knee to lock. In these cases, surgery may be needed, sometimes right away, to fix the flap or to remove the loose body.
Only when the majority of the meniscus is damaged beyond repair is the entire meniscus removed. This will significantly increase your risk of developing arthritis.
Preparations
What do I need to know before surgery?
You and Dr. Kiritsis should make the decision to proceed with surgery together. You need to understand as much about the procedure as possible. If you have concerns or questions, be sure and talk to Dr. Kiritsis.
Once you decide on surgery, you need to take several steps. Dr. Kiritsis may suggest a complete physical examination by your regular doctor. This exam helps ensure that you are in the best possible condition to undergo the operation.
You may also need to spend time with the physical therapist who will be managing your rehabilitation after surgery. This allows you to get a head start on your recovery.
One purpose of this preoperative visit is to record a baseline of information. The therapist will check your current pain levels, your ability to do your activities, and the movement and strength of each knee.
A second purpose of the preoperative visit is to prepare you for surgery. The therapist will teach you how to walk safely using crutches or a walker. And you’ll begin learning some of the exercises you’ll use during your recovery.
On the day of your surgery, you shouldn’t eat or drink anything after midnight the night before.
Surgical Procedure
What happens during meniscal surgery?
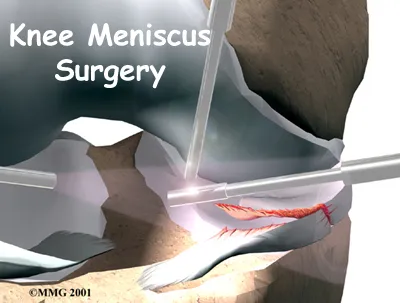
Meniscal surgery is done using an arthroscope, a small fiber-optic TV camera that is used to see and operate inside the joint. Only small incisions are needed during arthroscopy. Dr. Kiritsis does not need to open the knee joint.
Before surgery, you will be placed under either general anesthesia or a type of spinal anesthesia. Dr. Kiritsis begins the operation by making two or three small openings into the knee, called portals.
These portals are where the arthroscope and surgical instruments are placed inside the knee. Care is taken to protect the nearby nerves and blood vessels.
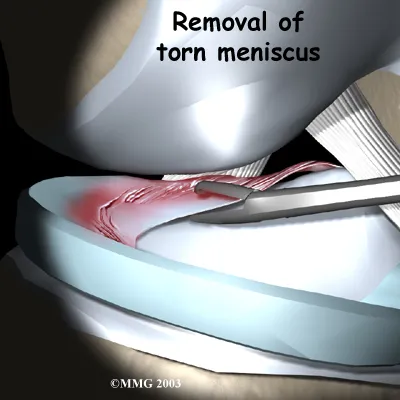
Partial Meniscectomy
The procedure to carefully remove a damaged portion of the meniscus is called partial meniscectomy. Dr. Kiritsis starts by inserting the arthroscope into one of the portals. A probe is placed into another portal. Dr. Kiritsis watches on a screen while probing the meniscus.
All parts of the inside of the knee joint are examined. When a meniscal tear is found, Dr. Kiritsis determines the type and location of the tear. Surgical instruments are placed into another portal and are used to remove the torn portion of the meniscus.
When the problem part of the meniscus has been removed, Dr. Kiritsis checks the knee again with the probe to be sure no other tears are present. A small motorized cutter is used to trim and shape the cut edge of the meniscus.
The joint is flushed with sterile saline to wash away debris from the injury or from the surgery. The portals are closed with sutures.
Meniscal Repair
Suture Repair
Using the arthroscope and a probe, Dr. Kiritsis locates the tear. The probe is used to push the torn edges of the meniscus together. A small rasp or shaver is used to roughen the edges of the tear. Then a hollow tube called a cannula is inserted through one of the portals. Dr. Kiritsis threads a suture through the cannula and into the knee joint. The suture is sewn into the two edges of the tear. The surgeon tugs on the thread to bring the torn edges close together. The suture is secured by tying two to three knots. Additional sutures are placed side by side until the entire tear is fixed.
An alternate method is to pierce the knee joint with one or two curved needles. The needle goes from the outer edge of the meniscus completely through the tear. Dr. Kiritsis may feed a suture from another portal into the end of the needle. Or the suture can be threaded into the needle from the outside of the knee. Both ways get the suture through the tear and allow Dr. Kiritsis to sew the torn edges of the meniscus together.
Suture Anchor Repair
Special fasteners, called suture anchors, are sometimes used to anchor the torn edges of the meniscus together. Suture anchors usually have a small piece of suture or plastic that deploys behind the meniscus and suture is attached that brings the two edges together.
Repairs using suture anchors work best for younger patients who have a single tear near the outer rim (red zone) of the meniscus. (As described earlier, this part of the meniscus has the richest blood supply.) A probe is often used to line up the torn edges of the meniscus. Then Dr. Kiritsis uses a small surgical tool to punch the anchor through the damaged part of the meniscus. Usually, only two or three anchors are needed. The anchors bring the two torn edges together while the tear heals.
Meniscal Transplantation
If the meniscus cannot be repaired or has been previously removed, a new form of treatment may offer a way to slow the onset of knee arthritis. Meniscal transplantation uses borrowed tissue to take the place of the original meniscus.
Experiments have been tried using various replacement materials. One material that is showing promise is an allograft. An allograft is a tissue that is from a donor, usually preserved human meniscus tissue. Because it is relatively new, this surgery is currently only available for select patients in a limited number of locations.
Using the arthroscope, the Dr. Kiritsis removes remnants of the old meniscus. Next, the allograft is prepared. Small sutures are placed around the edges of the allograft. Dr. Kiritsis slides the allograft with the sutures into the knee through a small incision.
The allograft is sewn in place onto the tibia bone. Surgical instruments, including a cannula or needle (described earlier), may be used to secure additional sutures. Some surgeons also use special anchors to firmly fix the allograft in place.
A probe is used to make sure the transplanted meniscus holds securely. The arthroscope is removed, and the portals are sewn shut.
Complications
What can go wrong?
As with all major surgical procedures, complications can occur. This document doesn’t provide a complete list of the possible complications, but it does highlight some of the most common problems. Some of the most common complications following meniscal surgery are
- anesthesia complications
- thrombophlebitis
- infection
- suture anchor problems
- graft failure
- slow recovery
- ongoing pain
Anesthesia Complications
Most surgical procedures require that some type of anesthesia be done before surgery. A very small number of patients have problems with anesthesia.
These problems can be reactions to the drugs used, problems related to other medical complications, and problems due to the anesthesia. Be sure to discuss the risks and your concerns with your anesthesiologist.
Thrombophlebitis (Blood Clots)
Thrombophlebitis, sometimes called deep venous thrombosis (DVT), can occur after any operation but is more likely to occur following surgery on the hip, pelvis, or knee. DVT occurs when blood clots form in the large veins of the leg.
This may cause the leg to swell and become warm to the touch and painful. If the blood clots in the veins break apart, they can travel to the lung, where they lodge in the capillaries and cut off the blood supply to a portion of the lung.
This is called a pulmonary embolism. (Pulmonary means lung, and embolism refers to a fragment of something traveling through the vascular system.) Dr. Kiritsis takes preventing DVT very seriously.
There are many ways to reduce the risk of DVT, but probably the most effective is getting you moving as soon as possible after surgery. Two other commonly used preventative measures include
- pressure stockings to keep the blood in the legs moving
- medications that thin the blood and prevent blood clots from forming
Infection
Following surgery, it is possible that the skin portals can become infected. This will require antibiotics and possibly another surgical procedure to drain the infection.
Suture Anchor Problems
Suture anchors can cause problems. If one breaks, the free-floating piece may hurt other parts inside the knee joint, particularly the articular cartilage. Also, the end of the anchor may poke too far through the meniscus. If so, the point may rub and irritate nearby tissues. A second surgery may be needed to fix problems with suture anchors.
Graft Failure
Surgeries where tissue is grafted into the body, like bone marrow or kidney transplants, have a high risk that the body will reject the graft. This is not so in meniscal transplant surgery. The preserved graft contains no live cells, so it doesn’t have to be matched up with the person getting the graft.
Also, the properties of meniscal tissue make rejection of a transplanted graft rare. The main reason for graft failure in meniscal transplant surgery occurs when patients try to do too much, too soon after surgery.
Doing sports where there are quick starts and stops, sharp pivoting, and jumping can cause the graft to fail. If the graft tears, another transplant surgery will be needed.
Slow Recovery
Not everyone after meniscal surgery gets quickly back to routine activities. Some people feel better and have less swelling, but they still find it hard to do normal activities even several months after surgery.
Others with damage in their knee ligaments or in the articular cartilage also tend to have a slower recovery. When an injury to the meniscus occurs, the shock absorption ability in the knee is compromised. This may lead to the progressive development of osteoarthritis.
Ongoing Pain
Pain relief does not always occur with meniscal surgery. If you have pain that continues or becomes unbearable, talk to Dr. Kiritsis about treatments that can help control your pain.
After Surgery
What happens after meniscal surgery?
Meniscal surgery is done on an outpatient basis. Patients go home on the same day as the surgery. The portals are covered with surgical strips, and the knee may be wrapped in an elastic bandage.
Crutches may be used after meniscal surgery. They may only be needed for one to two days after a simple meniscectomy. Dr. Kiritsis will specify how much weight can be borne after meniscal repair or allograft transplant.
Patients having meniscal repair are usually told not to place any weight on the foot for four to six weeks after surgery. After a transplant procedure, most patients are instructed to touch only the toes of the operated leg on the ground for four to six weeks.
Patients who have had a meniscal repair or transplant usually wear a knee brace for at least six weeks. The brace keeps the knee straight. It is removed often during the day to do easy range-of-motion exercises for the knee.
Follow Dr. Kiritsis’ instructions about how much weight to place on your foot while standing or walking. Avoid doing too much, too quickly. You may be told to use a cold pack on the knee and to keep your leg elevated and supported.
Rehabilitation
What will my recovery be like?
Your rehabilitation will depend on the type of surgery you had. You probably won’t need formal physical therapy after a partial meniscectomy. Most patients can do their exercises as part of a home program.
If you require outpatient physical therapy, you will probably need to attend therapy sessions for two to four weeks. You should expect full recovery to take up to three months.
Dr. Kiritsis will have you take part in formal physical therapy after meniscal repair and transplant procedures. The first few physical therapy treatments are designed to help control the pain and swelling from the surgery. Physical therapists will also work with patients to make sure they are putting only a safe amount of weight on the affected leg.
For the first four to six weeks after a meniscal repair, you may be instructed to avoid bending the knee more than 90 degrees. Then it is safe to gradually bend the knee fully. However, you should avoid squatting for at least three to four months while the repair fully heals.
It is not advisable to run, jump, or twist the knee for at least four to six months. Patients sometimes resume sports activities within four to six months after surgery to repair the meniscus.
Range-of-motion exercises start right away after a transplant. The goal is to get the knee to bend to 90 degrees within four weeks after surgery. As time goes on, more challenging exercises are chosen to safely advance the knee’s range of motion, strength, and function.
Ideally, patients will be able to resume their previous activities. Some patients may be encouraged to modify their activity choices, especially if an allograft was used.
The physical therapist’s goal is to help you keep your pain under control and improve your knee’s range of motion and strength. When you are well under way, regular visits to your therapist’s office will end. The therapist will continue to be a resource, but you will be in charge of doing your exercises as part of an ongoing home program.


Paul G. Kiritsis, MD
Dr. Kiritsis, a Richmond native, is one of a select number of Orthopedic Surgeons in the Richmond area to hold a second subspecialty board certification in Sports Medicine.

