A patellar tendon rupture happens when the tendon connecting your kneecap to your shinbone tears, leading to intense knee pain and difficulty straightening the leg. This post explains the causes, symptoms, and treatment options for patellar tendon rupture.
Key Takeaways
- Patellar tendon ruptures are typically acute resulting from high-stress activities impacting the knee, and they significantly affect knee function.
- Diagnosis involves a combination of medical history, physical examination, and possibly imaging tests to determine if the tear is partial or complete, guiding treatment options.
- Treatment varies between partial tears, which often respond well to conservative methods like physical therapy, and complete tears, which require surgical intervention for optimal recovery.
Understanding Patellar Tendon Rupture
A patellar tendon rupture is a complete tear of the tendon that connects your kneecap (patella) to your shinbone (tibial tubercle). These ruptures can be categorized into acute patellar tendon rupture and chronic patellar tendon partial tears. Acute tears typically result from a sudden, high-stress event, while chronic tears develop over time due to repeated stress and tendon degeneration. Additionally, a ruptured patella tendon can lead to significant impairment in knee function.
Patellar tendon ruptures often occur during activities that place a high load on the knee’s extensor mechanism, such as running up stairs, landing from a jump, or making abrupt direction changes. This injury is particularly common in men aged 30-40, often disrupting the distal aspect of the extensor mechanism. Imagine running up a flight of stairs, feeling a sudden pop, and then being unable to straighten your knee – that’s the hallmark of a patellar tendon rupture.
The patellar tendon connects the patella to the tibial tubercle and plays a critical role in knee extension and resisting knee flexion. When this tendon tears, the quadriceps tendon pulls the kneecap higher than normal, a condition known as patella alta.
Anatomy of the Patellar Tendon
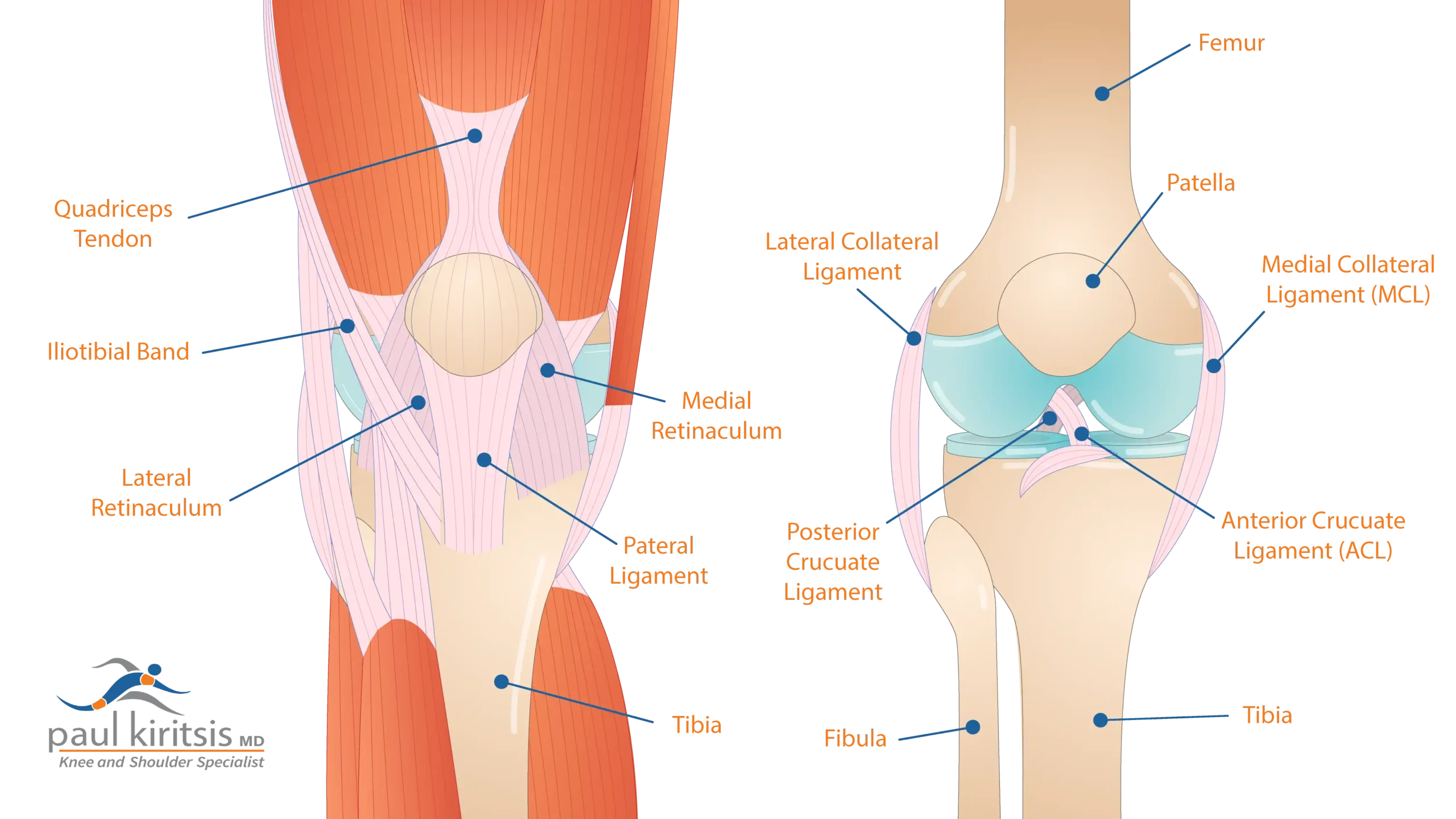
Understanding the anatomy involved is helpful to fully grasp the implications of a patellar tendon rupture. The patellar tendon acts as a pivotal link between the quadriceps muscle and the tibia, facilitating knee extension. The quadriceps muscles group, located at the front of your thigh, is the primary initiator of the knee’s extensor mechanism. This group of muscles generates the force needed to straighten your leg, with the patellar tendon transmitting this force to the shinbone.
Additionally, the patellar tendon consists of retinacula that converge to provide further stability to the knee joint. This anatomical setup ensures that the knee can perform complex movements efficiently. Most patellar tendon tears occur at the proximal end, where the tendon attaches to the kneecap.
Causes and Risk Factors
Patellar tendon ruptures can be caused by various factors, ranging from direct impacts to overuse injuries. Direct impacts from falls, landings, or jumping are common causes of these ruptures.
Overuse injuries, where the tendon is subjected to repetitive stress, can also lead to rupture. Conditions such as tendinitis, degeneration, and systemic diseases like diabetes and lupus weaken the patellar tendon, making it more susceptible to rupture.
Risk factors such as age, previous injuries, and underlying health conditions significantly increase the chances of experiencing a patellar tendon rupture.
Symptoms of Patellar Tendon Rupture
Recognizing the symptoms of a patellar tendon rupture is key to seeking timely medical help. When a rupture occurs, you may feel a pop, followed by intense pain and swelling just below the kneecap. This pain can be debilitating, making it difficult to move or bear weight on the affected leg.
In addition to knee pain, a noticeable indentation or ‘divot’ may be felt below the kneecap, contributing to significant knee instability and difficulties in walking. This physical sign, combined with swelling and tenderness, is a strong indicator of a patellar tendon rupture. For those with a complete tear, the inability to fully straighten the knee is a telltale sign, indicating a significant loss of function.
These symptoms can severely impact daily activities and athletic performance. Seek medical evaluation if you experience such symptoms to confirm the injury and start appropriate treatment.
Diagnosis of Patellar Tendon Rupture
Diagnosing a patellar tendon rupture involves a combination of medical history, physical examination, and imaging tests. A thorough medical history interview will help the orthopedic surgeon understand your general health, symptoms, and any preceding events that might have led to the injury. This is followed by a detailed physical examination of the knee to assess the extent of the damage.
Clinically recognized signs of a patellar tendon tear include a palpable defect, tenderness, and the inability to extend the knee. The knee extension test is a common diagnostic tool used to confirm a patellar tendon tear. Imaging tests such as X-rays can reveal the displacement of the kneecap, while MRI provides a detailed visualization of soft tissue injuries, including the extent of the tear and patellar tendon tear symptoms.
Ultrasonography is another useful tool for assessing the condition of the patellar tendon, offering a cost-effective alternative to MRI. These diagnostic methods collectively offer a comprehensive understanding of the injury, guiding effective treatment plans.
Partial vs. Complete Tears
Patellar tendon tears can be classified as partial or complete, each requiring different treatment approaches. Partial tears involve only a portion of the tendon being damaged, often resulting in pain and limited knee function but not a complete loss of movement. These tears can typically be managed with nonsurgical treatments like immobilization, assistive braces, physical therapy, and PRP injections.
In contrast, a complete patellar tendon tear means the tendon is fully separated from the kneecap, leading to significant functional loss and the inability to straighten the knee. This complete rupture necessitates surgical intervention to reattach the tendon. Understanding the severity of the tear is crucial for determining the appropriate treatment plan.
Nonsurgical treatments are effective for partial tears, focusing on rest, immobilization, and rehabilitation exercises to restore strength and flexibility. On the other hand, immediate surgical repair is usually required for complete tears to ensure proper healing and regain full knee function.
Conservative Treatment Options
Conservative treatment options are highly effective for partial patellar tendon tears. Rest and immobilization with braces or splints are often the first steps in managing these injuries. This immobilization period usually lasts up to six weeks, allowing the tendon to heal. During this time, pain relief can be achieved through medication management and ice massage to reduce inflammation and soreness, which is crucial before considering acute patellar tendon repair.
Physical therapy plays a vital role in the recovery process, starting with gentle movements to prevent stiffness and progressing to more intensive strengthening exercises as healing advances. Cross-friction massage can also improve blood circulation to the tendon area, enhancing flexibility and promoting recovery.
Regular stretching and maintaining proper technique during physical activities are essential to avoid undue stress on the joints. Following these conservative treatment options often allows individuals with partial patellar tendon tears to return to their normal activities without surgical intervention. PRP injections may also be used to aid with discomfort and facilitate healing.
Surgical Treatment for Complete Ruptures
When it comes to complete patellar tendon ruptures, surgical treatment is necessary to restore knee function. Surgery is required because nonsurgical options are limited in addressing the complete separation of the tendon from the kneecap. Prompt surgical intervention is important, especially for acute ruptures, to avoid complications associated with delayed treatment.
The type of surgical intervention depends on the rupture’s location and severity. Primary repair works well for acute ruptures. However, chronic cases might need tendon reconstruction. Surgical techniques can include transosseous tendon repair and suture anchor tendon repair, each tailored to the specific needs of the patient.
Despite the potential risks such as infections and wound issues, timely and effective surgical treatment significantly improves outcomes. Surgery is necessary for individuals with complete patellar tendon tears. This procedure helps them regain full knee function and resume their normal activities.
Postoperative Care and Rehabilitation
Rehabilitation after surgery is critical for restoring knee function and strength, particularly after patellar tendon repair. Patience will typically begin range of motion shortly after surgery. We normally allow them to bend their knee to 30° and progress 10° per week to achieve 90° by six weeks. Furthermore, patience can begin to touch weight-bearing with their knee brace locked in extension after surgery. We will, progress them to full weight-bearing locked extension at four weeks and the brace will be unlocked for ambulation at six weeks. We typically discontinue the brace at eight weeks.
From weeks 6 through 12, the rehabilitation focus shifts to normalizing gait on flat surfaces and beginning active quadriceps contraction. Gradual progression from passive to active knee movements is crucial in the recovery process. Physical therapy plays a key role in restoring strength and range of motion, incorporating exercises like isometric quadriceps exercises and proprioceptive training to enhance balance and coordination.
Full mobilization, concentric, and eccentric exercises, as well as non-impact balance drills, are included in the later stages of rehabilitation. A multidisciplinary approach involving physical therapists and orthopedic specialists can significantly enhance recovery outcomes. A structured rehabilitation program helps patients achieve successful recovery and return to their normal activities.
Recovery Timeline
The recovery timeline for patellar tendon ruptures can vary depending on the severity of the tear and the treatment approach. For partial tears, the knee may need to be immobilized for up to six weeks, with a full return to activity expected around 3-4 months.
The recovery process for complete tears can take several months to a year, with significant strength and functionality typically regained by 16 weeks post-surgery. The expected return to sport timeline after surgery for patellar tendon ruptures is around six months postoperatively. Understanding this timeline helps set realistic expectations for patients and caregivers, ensuring a smooth recovery process.
Complications and Prognosis
Untreated patellar tendon ruptures can lead to complications such as altered knee range of motion, early fatigue, patellofemoral pain, instability and an inability to ambulate. Poor outcomes after surgery can be linked to missed or delayed diagnoses. Additionally, treatment errors and technical mistakes during the repair process can contribute to these negative results. However, with timely intervention, the prognosis for most patients is excellent, with high rates of return to activity.
Preventive Measures
Preventive measures are important for maintaining knee health and avoiding significant injuries like patellar tendon ruptures. Strength training can improve the resilience of the patellar tendon, reducing the risk of rupture during physical activities. Proper conditioning, including flexibility and stability exercises, plays a key role in tendon health and injury prevention.
Avoiding activities that excessively strain the patellar tendon, such as high-impact sports without adequate preparation, is helpful for prevention. Incorporating these preventive measures into your routine significantly lowers the risk of patellar tendon injuries and helps maintain optimal knee health.
Summary
Understanding patellar tendon ruptures, their causes, symptoms, and treatment options is crucial for effective management and recovery. Whether dealing with partial or complete tears, timely diagnosis and appropriate treatment can significantly improve outcomes. Conservative treatments can be effective for minor injuries, while surgical intervention is necessary for complete ruptures.
The recovery process involves careful rehabilitation and gradual reintroduction of activities, with a focus on restoring strength and function. Preventive measures, such as strength training and proper conditioning, are essential for maintaining knee health and avoiding future injuries. With the right knowledge and approach, you can tackle patellar tendon ruptures and return to your normal activities with confidence.
Frequently Asked Questions
What are the common symptoms of a patellar tendon rupture?
A patellar tendon rupture commonly presents with a popping sensation, intense pain below the kneecap, noticeable swelling, a visible indentation beneath the kneecap, and difficulty in fully straightening the knee. Prompt medical evaluation is essential for an accurate diagnosis and appropriate treatment.
How is a patellar tendon rupture diagnosed?
A patellar tendon rupture is diagnosed through a comprehensive assessment including medical history, physical examination, and imaging tests like X-rays and MRI to evaluate the extent of the injury. These steps ensure an accurate understanding of the tendon tear and any associated damage.
What is the difference between partial and complete patellar tendon tears?
Partial patellar tendon tears involve damage to only a segment of the tendon, often treated with non-surgical methods, while complete tears signify total detachment from the kneecap, necessitating surgery for repair.
What does the postoperative rehabilitation process look like for a patellar tendon rupture?
The postoperative rehabilitation process for a patellar tendon rupture includes initial immobilization, controlled weight-bearing exercises, and a gradual progression from passive to active knee movements, alongside physical therapy to restore strength and range of motion. This comprehensive process typically spans several months.
How can I prevent a patellar tendon rupture?
To prevent a patellar tendon rupture, focus on strength training to enhance tendon resilience and incorporate flexibility and stability exercises into your routine. Additionally, ensure you prepare properly before engaging in high-strain activities.





