Can a meniscus tear heal on its own? It’s a question that plagues many facing this common knee injury. While some meniscus tears have the capacity for self-repair, especially those with adequate blood supply, others may require surgical intervention.
This post will guide you through the factors affecting the healing of a meniscus tear, outlining when conservative treatments could suffice and when surgery becomes a necessity.
Key Takeaways
- The meniscus, a critical structure in the knee, has a complex blood supply that varies across different zones, influencing the natural healing ability of a meniscus tear.
- Meniscus tears are categorized into traumatic, often sport-related, and degenerative, associated with aging; their healing potential varies based on the type, size, and location of the tear.
- Treatment for meniscus tears ranges from non-surgical options like the RICE method, medications, and physical therapy to surgical interventions, with the approach depending on factors such as tear severity, patient age, and knee function.
Understanding the Meniscus
The crescent-shaped meniscus, often likened to the knee’s shock absorber, is a marvel of bioengineering designed to:
- withstand the everyday rigors of bearing weight and facilitating movement
- cushion the joint
- enhance stability, ensuring that each step you take isn’t a jarring jolt to your system
The importance of the meniscus cannot be overstated—it’s a linchpin in the orchestra of knee function, and when it succumbs to injury, the symphony of movement can quickly become a cacophony of pain.
Upon examining the anatomy of these vital knee components, we discover two menisci comfortably nestled between the thigh bone (femur) and shin bone (tibia), each accurately positioned to distribute the forces that our legs face daily. The meniscus is a meniscal structure that spans from the medial meniscus, robustly seated on the knee’s inner edge, to the lateral meniscus, gracing the outer boundary. Together, they form a dynamic duo that, when intact and healthy, makes activities from sprinting to stooping seamless and pain-free.
The Importance of the Meniscus
Imagine the meniscus as the knee’s unsung hero: a guardian against the relentless wear and tear that threatens the joint’s integrity. With every step, jump, or pivot, the menisci distribute stress evenly, sparing the knee from the damage that could lead to arthritis or other debilitating conditions. They’re the gatekeepers of knee function, compensating for instability, aiding in load transmission, and ensuring that everything from a gentle walk to an explosive leap feels effortless.
However, these protectors are not immune to damage; a meniscus tear has the potential to disrupt the knee’s biomechanics, leading to a range of problems from diminished proprioception to heightened joint stress. Without the menisci, the load on the knee joint becomes concentrated on a smaller area, elevating the risk of cartilage damage and hastening the onset of joint degeneration. This articulates the critical need for prompt and effective treatment, emphasizing the significance of the menisci’s role in maintaining knee health and function.
Anatomy of the Meniscus
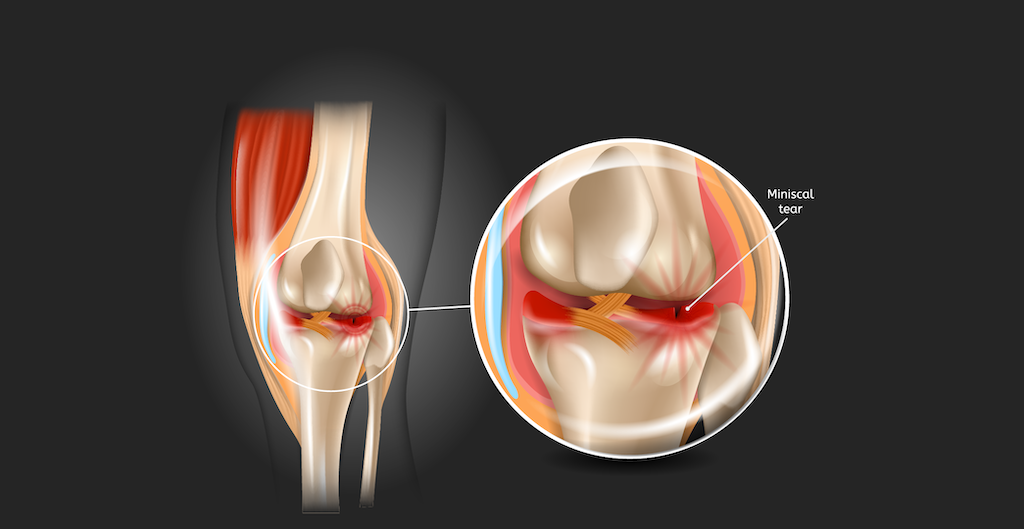
A more detailed look into the meniscus uncovers a complex anatomy closely linked to the knee’s performance. The medial meniscus, a steadfast presence on the inside of the knee, and the more mobile lateral meniscus on the outside, are not mere passive structures—they’re anchored to the leg muscles and connected to the knee’s ligaments, forming a network that responds to the knee’s every move. This interconnectivity contributes to the knee’s overall stability, allowing for fluid knee motion that’s free from restriction or discomfort.
The menisci’s ability to perform these vital functions hinges on their blood supply, stemming from the inferior genicular artery. This vascular lifeline is crucial in delivering the nutrients required for tissue repair and maintenance. However, not all regions of the meniscus are created equal in terms of blood flow—some areas are well-nourished, while others are less fortunate, a disparity that plays a significant role in the healing prospects of meniscus tears.
Causes and Types of Meniscus Tears
Whether resulting from an aggressive twist during an intense basketball game or the accumulated consequences of years of daily wear and tear, meniscus tears come in various forms, each with its own unique narrative. Broadly categorized into traumatic and degenerative types, these most common knee injuries can stem from a variety of causes—some as dramatic as an athletic knee injury, others as subtle as the gradual wear and tear of aging. Understanding these distinctions is key to tailoring treatment and setting realistic expectations for recovery.
Traumatic meniscus tears often serve as the antagonists in many athletes’ stories, occurring when the knee is twisted or bent under strain, frequently during intense competition or an abrupt change in direction. Conversely, degenerative meniscus tears are more insidious, manifesting quietly over time as the meniscus succumbs to the inevitable passage of time and the wear that accompanies it. Each type of tear presents unique challenges and requires a nuanced approach to treatment.
Traumatic Meniscus Tears
Picture an athlete in full flight, making a sudden pivot, when an unexpected pop in the knee brings everything to a standstill. This is the hallmark of a traumatic meniscus tear, an injury that spares no one—whether it’s a seasoned pro or a weekend jogger. Activities that place high demands on the knee, such as deep squatting, heavy lifting, or aggressive pivoting, are common precursors to these severe tears. And it’s not just the domain of contact sports; even non-contact activities that involve rapid starts and stops can pose a risk.
The patterns of traumatic tears – longitudinal, radial, and the feared bucket-handle – narrate the story of the impact and direction of the injury. These tears are not just painful; they threaten the very function of the knee, potentially leading to instability and a compromised ability to bear weight. It’s a stark reminder of the knee’s vulnerability and the need for preventative measures and prompt medical attention when injury strikes.
Degenerative Meniscus Tears
As time progresses, the risk of a degenerative meniscus tear escalates, proving that time does not spare anyone – not even our sturdy menisci. These tears are the result of the gradual breakdown of the meniscal structure over the years, often without a dramatic event to signal their onset. A simple twist or an awkward step can be enough to cause a tear in the brittle, aged tissue of the meniscus, leading to pain and limited knee motion that can impede even the most basic of daily activities.
While younger individuals might bounce back from a meniscus injury with relative ease, older adults may find themselves weighing the pros and cons of conservative treatments versus the possibility of surgery. Degenerative tears often call for a more patient, methodical approach to treatment, one that respects the delicate balance between healing and the ongoing demands placed on aging knees. It’s a delicate dance of managing symptoms and maintaining knee function, all while acknowledging the complex interplay of age, activity, and anatomy.
Symptoms and Diagnosis of a Torn Meniscus
When a meniscus tear enters the picture, it announces its presence with symptoms that can range from mildly inconvenient to downright debilitating. The hallmark signs of a meniscus tear include:
- Knee pain
- A sensation of weakness or instability
- Swelling
- Feeling of the knee locking or catching
These symptoms are red flags that something isn’t quite right in the intricate workings of the knee joint. It’s a clarion call for medical attention, a signal that the knee’s inner harmony has been disrupted.
But recognizing symptoms is just the first step; confirming a diagnosis of a meniscus tear is an endeavor that requires more than just a keen eye and a description of pain. Healthcare professionals turn to a battery of diagnostic methods to peer beneath the skin and into the knee’s inner sanctum, where the true nature of the injury can be revealed. It’s a journey from the subjective experience of pain to the objective clarity of medical imaging.
Common Symptoms
When a meniscus tear strikes, it doesn’t whisper—it yells. The pain, often sharp and localized to the inner or outer side of the knee, can be a constant companion, flaring up with certain movements or even at rest. Swelling and stiffness in the knee are common co-conspirators, making every bend and extension a challenge, and potentially leading to a reduced range of motion that can hamper even the simplest of tasks.
But it’s the sensations of locking or catching that truly unsettle, transforming the knee into an erratic joint that can’t be trusted to perform when needed. These symptoms aren’t just discomforts; they’re impediments to mobility and independence, turning every step into a potential ordeal. They’re the body’s way of sounding the alarm, signaling the need for prompt evaluation and treatment to restore the knee’s smooth operation.
Diagnostic Methods
Navigating the road to a meniscus tear diagnosis is a task for the experts—physiatrists, primary care sports medicine physicians, and orthopedic surgeons with a penchant for puzzles and a deep understanding of the knee’s anatomy. The physical examination is their first tool, a hands-on approach that assesses the knee’s structure and function, searching for signs of damage by manipulating the joint and observing the gait. It’s a blend of art and science, where experience and intuition meet the tangible evidence of injury.
Yet, the physical examination is just a prelude to the imaging tests that bring the hidden details of the knee into sharp relief. X-rays, while unable to visualize the soft tissues directly, serve as sentinels, ruling out other conditions that might masquerade as a meniscus tear. MRI scans are the gold standard, creating a detailed portrait of the knee’s interior landscape, highlighting the precise location and severity of the tear. With this high-resolution roadmap, a definitive diagnosis is within reach, paving the way for a targeted, effective treatment plan.
Factors Affecting Meniscus Tear Healing
Commencing the healing journey post a meniscus tear is not a universal process. Multiple factors come into play, influencing the body’s capacity to repair the damaged tissue and determining the treatment course. The meniscus’s delicate blood supply, the specific location of the tear, and its severity all converge to either facilitate natural healing or necessitate a more interventional approach. It’s a complex interplay of biological variables that can make or break the healing process.
For those who prefer a more organic recovery or wish to steer clear of the strenuousness of surgery, comprehension of these factors is vital. Simple daily activities and gentle exercises might be within reach, but only if they don’t aggravate the injury further. It’s a balancing act, requiring patience and prudence to navigate the fine line between activity and rest, between giving the body the time it needs to heal and keeping the knee agile and strong.
Blood Supply and Tear Location
The healing potential of the meniscus is intimately connected with its blood supply – or the absence of it. The so-called “red zone” of the meniscus, rich in blood vessels, offers hope for tears that occur within its borders, as the abundant blood flow brings with it the necessary cells for repair. The “white zone,” on the other hand, is a desolate landscape for healing, its avascular nature rendering it incapable of mending the rifts that form within it. And then there’s the “red-white zone,” a transitional area where the healing potential falls somewhere in the middle, neither rich nor entirely barren.
It’s an unfortunate truth that not all tears are created equal; those that occur in the white zone often have no choice but to seek refuge in surgery, given the area’s inability to mount an effective healing response. The location of the tear, therefore, becomes a crucial determinant in the decision-making process, guiding patients and healthcare providers alike as they chart the course between conservative management and surgical intervention.
Severity of the Tear
The size and complexity of a meniscus tear can be as varied as the individuals who suffer from them, and these characteristics are pivotal in determining a tear’s fate. Smaller, less complicated tears that reside in the vascular zones of the meniscus carry the torch of hope, their healing prospects brighter than their more severe counterparts. The body’s inherent repair mechanisms might suffice to mend these minor injuries, avoiding the need for surgical measures.
However, the recovery timeline is not a short sprint; it’s a marathon that can stretch from a mere four weeks for minor tears to a daunting eight weeks or more for the more severe or complex cases. Healing is not merely a passage of time; it’s an intricate biological process that can be influenced by factors such as the patient’s age, overall knee health, and the presence of other joint issues. The severity of the tear, thus, becomes a lighthouse guiding the way through the fog of treatment options, illuminating the path to recovery—be it through natural healing or the helping hand of surgery.
Non-Surgical Treatment Options for Meniscus Tears
Not all meniscus tears necessitate the dramatic intervention of surgery; many find comfort in the softer approach of non-surgical treatments. These conservative measures are the first line of defense against the discomfort and dysfunction that accompany a torn meniscus, offering a less invasive path to recovery that can be both effective and appealing for those wishing to avoid the operating room. Some non-surgical treatment options, which can help a torn meniscus heal, include:
- The RICE method (Rest, Ice, Compression, Elevation)
- Physical therapy
- Pain medication
- Steroid injections
These treatment options cater to the body’s natural healing abilities.
The appeal of non-surgical treatment is not only due to its less invasive character but also its emphasis on enabling the body to heal itself. Minor tears, especially those that occur in the younger population or within the more vascular areas of the meniscus, stand a good chance of healing under the watchful care of conservative treatment. It’s a journey marked by patience and perseverance, where the body is given the time and support it needs to weave together the frayed edges of the meniscus and help the meniscus tear heal.
Conservative Measures
The journey towards healing a meniscus tear commences with the reliable RICE method – Rest, Ice, Compression, and Elevation. This quartet works in concert to soothe the injured knee, calming inflammation and providing the tranquil environment needed for the meniscus to begin mending. Rest, in particular, is a cornerstone of this approach, allowing the knee to recuperate from the stress and strain that may have contributed to the tear. By stepping away from activities that exacerbate the injury, patients can manage pain and prevent further damage to the already fragile meniscal tissue.
When it comes to pain management, nonsteroidal anti-inflammatory medications such as ibuprofen and naproxen are valuable allies, offering relief from the discomfort and swelling that often accompany a meniscus injury. In some cases, corticosteroid injections may be called upon to reduce inflammation more directly, providing a respite from pain and facilitating a smoother rehabilitation process. It’s a balancing act of providing enough support to the knee without overburdening it, a delicate dance that steers the knee away from the operating table and towards a natural recovery.
Physical Therapy and Rehabilitation
Once the initial inflammation lessens, physical therapy becomes the primary focus in the non-surgical treatment of a meniscus tear. It’s a process that isn’t just about healing—it’s about retraining, strengthening, and preparing the knee for the rigors of daily life. Tailored exercise programs target the muscles surrounding the knee, building a robust support system that can alleviate the burden on the healing meniscus. It’s a form of empowerment, where patients actively participate in their own recovery, guided by the expertise of physical therapists.
The exercises prescribed are varied and purposeful, each one carefully chosen to foster muscle strength and flexibility without putting undue stress on the injured meniscus. Patients engage in a variety of activities, including:
- Quadriceps setting
- Hamstring curls
- Leg extensions
- Stationary biking
This creates a well-rounded regimen that promotes healing and functional improvement. This phase can last anywhere from a few weeks to a couple of months, depending on the severity of the tear and the individual’s response to therapy. It’s a journey of incremental progress, where each step forward is a victory in the quest to regain a pain-free, fully functional knee.
When Surgery is Necessary
Despite the utmost efforts of non-surgical treatments, there are instances where the meniscus damage is too intense or the tear location too risky for natural healing to be a feasible choice. Surgery may become the beacon of hope for those whose tears are situated in the bloodless realms of the white zone or for those who continue to suffer symptoms despite exhaustive conservative measures. It’s a decision not taken lightly, often the culmination of careful evaluation and consideration of the patient’s lifestyle, age, and overall knee health.
The idea of surgery can be intimidating, but for some, it signifies the most straightforward route to restoring knee function and returning to an active life devoid of pain. Younger individuals and those with physically demanding routines may find surgical repair especially compelling, as it promises a quicker and more reliable return to full mobility compared to conservative treatment alone. In the hands of skilled orthopedic surgeons, using advanced techniques and a minimally invasive approach, surgery can repair the tear and set the stage for a robust recovery.
Types of Surgical Procedures
When meniscal surgery is considered, the type of procedure selected is customized to the distinct characteristics of the meniscus tear. Arthroscopic surgery is the go-to technique, a minimally invasive approach that allows surgeons to repair the meniscus with accuracy and minimal disruption to surrounding tissues. Through tiny incisions, specialized instruments are introduced into the knee joint, enabling the surgeon to remove damaged tissue or, more ideally, to suture and repair the meniscus, preserving as much of the natural structure as possible.
The specific methods of meniscus repair—inside-out, outside-in, and all-inside—each come with their own set of advantages and are selected based on the tear’s location and pattern. In more severe cases, where much of the meniscus has been removed or damaged beyond repair, a meniscus transplant using donor tissue may be the best course of action. This procedure offers new hope for patients seeking to regain the full function of their knee, inviting a fresh start for a joint that has been compromised by injury.
Recovery After Surgery
The journey doesn’t conclude with surgery; in truth, the postoperative rehabilitation significantly shapes the recovery experience. The timeline for regaining knee function varies dramatically, hinging on whether the surgery involved trimming away torn meniscus tissue or repairing the tear with sutures. Procedures like partial meniscectomy typically allow for a quicker return to activity, often within three to six weeks, while more extensive meniscus repairs necessitate a longer period of healing, potentially taking up to six months before full function is restored.
Physical therapy remains a cornerstone of the post-surgery recovery process, as vital as the surgery itself. It’s a time of rebuilding and reeducation, where patients work closely with physical therapists to gradually restore strength, flexibility, and range of motion. Exercises and activities are introduced progressively, ensuring the knee is not overtaxed too soon, all with the goal of returning to a level of activity that is both satisfying and sustainable.
It’s a period marked by patience and determination, as each day brings the patient one step closer to a fully healed knee.
Summary
In the intricate dance between the knee’s form and function, a meniscus tear can disrupt the rhythm, leading to pain, immobility, and a pressing need for effective treatment. From understanding the essential role of the meniscus and recognizing the signs of a tear to exploring the factors that influence healing and the spectrum of treatment options, we’ve delved into the complex narrative of meniscus injury and recovery.
Whether through the natural healing enabled by conservative measures or the precise intervention of surgery, the goal remains the same: to return the knee to its former glory, enabling a return to the activities that enrich our lives.
Frequently Asked Questions
What is meniscus?
The meniscus is a C-shaped piece of cartilage that acts as a cushion between the shinbone and thighbone in the knee, and it can tear due to forceful twisting or rotation.
What are 3 signs of a meniscus tear in the knee?
If you experience a popping sensation, swelling or stiffness, and pain when twisting or rotating your knee, it could be a sign of a meniscus tear. Difficulty straightening the knee and a “locked” feeling are also common signs.
What happens if a meniscus tear is left untreated?
If left untreated, a meniscus tear can result in pain, reduced mobility, and potential need for serious surgeries in the future. It’s important to seek proper treatment to avoid these complications.
Is walking good for torn meniscus?
If you have an acute tear, walking may be possible with minimal discomfort, but it’s best to avoid it if you experience increased pain or have a severe tear. Always follow your doctor’s advice and be cautious with movements that could worsen the tear or cause pain.
How long does it take for a torn meniscus to heal without surgery?
Without surgery, a torn meniscus takes about 6 to 8 weeks to heal. If symptoms persist after 3 months or become significant, surgery may be recommended.




