Glenoid fractures, though relatively uncommon, represent a significant injury to the shoulder joint that can have lasting impacts on mobility and function if not properly treated.
The glenoid is the socket portion of the shoulder’s ball-and-socket joint, and fractures here often result from high-energy trauma such as motor vehicle accidents, falls, or sports injuries. Because of the complex anatomy and the vital role the glenoid plays in shoulder stability, these fractures require careful diagnosis and a tailored treatment approach.
In this post, we’ll explore the causes, classification, diagnosis, and management options for glenoid fractures, shedding light on a topic that’s often overlooked in orthopedic discussions.
Key Takeaways
- Glenoid fractures, although rare, can significantly impact shoulder stability and function, often resulting from high-energy trauma or low-impact falls in the elderly.
- Accurate diagnosis of glenoid fractures relies on a combination of physical examination and advanced imaging techniques, with CT scans being the gold standard.
- Surgical treatment is indicated for displaced fractures, with arthroscopic techniques emerging as a minimally invasive option that enhances recovery and reduces complication rates.
Understanding Glenoid Fractures
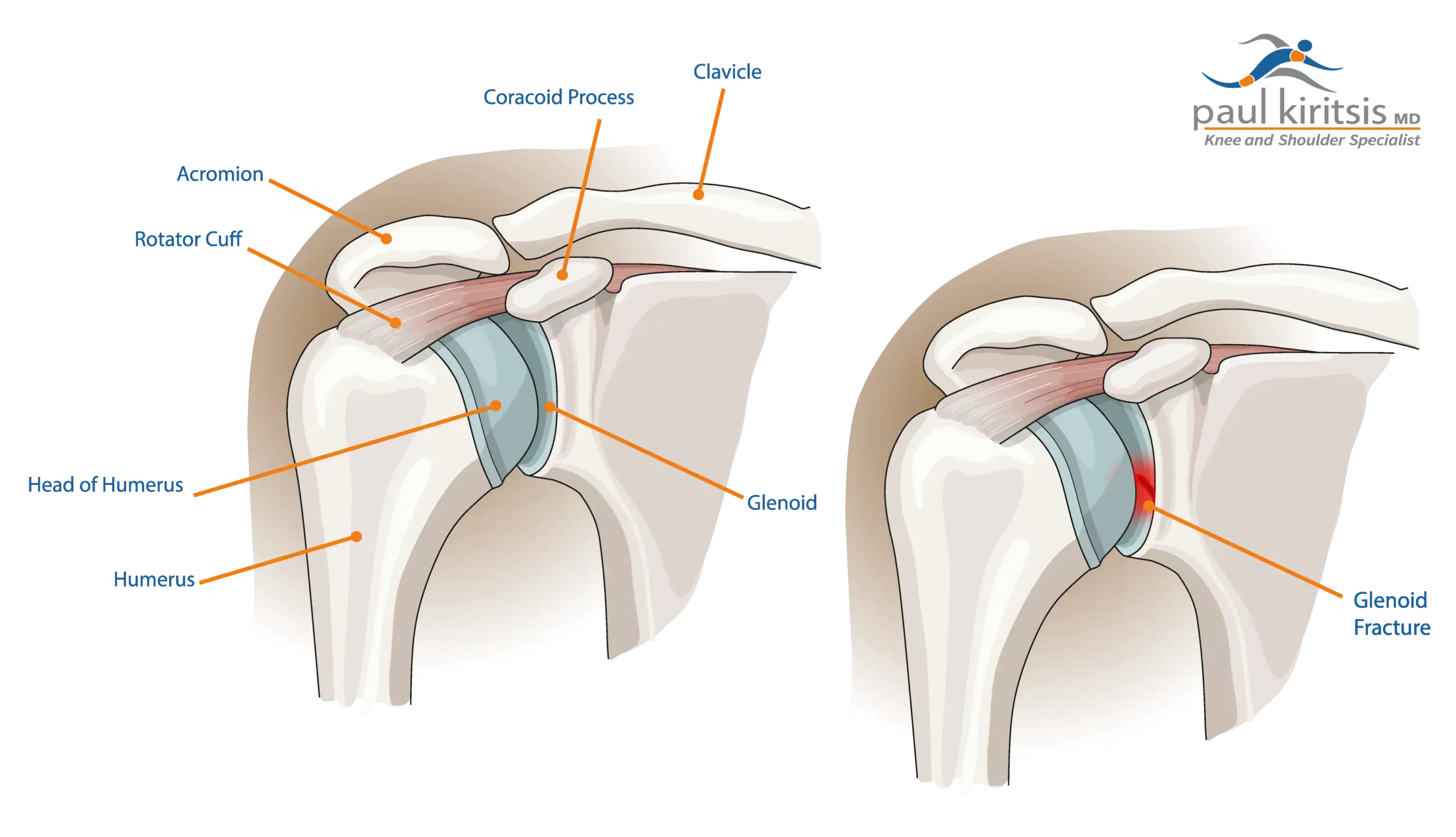
The glenoid cavity, a shallow dish-shaped structure located on the lateral scapula, plays a pivotal role in stabilizing the humeral head within the ball-and-socket shoulder joint. However, its pear-shaped or oval fossa, combined with the thinner and steeper anterior vault, makes it susceptible to instability and fractures. Despite their uncommon nature, these fractures demand attention due to their potential impact on shoulder stability and function.
Typically resulting from high-energy trauma such as vehicular accidents or falls, glenoid fractures can also occur from low-impact falls in elderly patients. Symptoms usually include pain, swelling, and limited mobility, which are common indicators that necessitate further investigation.
How Glenoid Fractures Are Diagnosed
Diagnosing a glenoid fracture involves both a careful physical exam and the use of imaging tests. X-rays are usually the first step, especially special views that help doctors see the socket of the shoulder more clearly. However, a CT scan is often needed to get a much more detailed look at the fracture. In many cases, 3D images created from the CT scan can show exactly how the bone is broken, which helps in planning the best treatment.
During the physical exam, your doctor will check your shoulder, upper arm, and nearby bones to see how well you can move, whether you have any weakness, and to make sure your nerves and blood vessels are working properly. Understanding how the injury happened—like a fall or car accident—can also help pinpoint the type of fracture you have.
Getting a prompt evaluation by an orthopedic surgeon who specializes in shoulders is important. Accurately identifying the type of fracture leads to better treatment choices and improved recovery.
Classifying Glenoid Fractures
Shoulder surgeons use classification systems to better understand and treat glenoid fractures. These systems help describe where the fracture is, how severe it is, and whether it affects the shoulder joint itself. Think of it like organizing different types of breaks into categories to guide the best treatment plan.
One of the most commonly used systems is called the Ideberg classification. It divides glenoid fractures into six main types based on where the break is in the socket. For example, one of the most frequent injuries is a Type Ia fracture, which affects the front edge of the socket and often happens when the shoulder is dislocated.
Another system, developed by the AO Foundation, looks at the overall structure of the scapula (shoulder blade) and how much the joint is involved. There’s also a newer system called the Clause classification, which includes a wider range of fracture types, such as breaks in the body of the scapula or those that go into the joint surface.
These classification systems are important because they help doctors choose the most effective treatment. As our understanding of shoulder injuries improves, these systems continue to evolve—leading to better care and recovery for patients like you.
When Is Surgery Needed for a Glenoid Fracture?
Not all glenoid fractures need surgery—but in some cases, it’s the best option to help your shoulder heal properly and regain full function. Surgery is usually recommended when the broken pieces of bone are out of place (called displacement) or if the shoulder joint becomes unstable because of the fracture.
One key reason for surgery is if the surface of the socket is uneven by more than 5 millimeters. Another common reason is when more than 25% of the joint surface is involved in the break. These issues can affect how your shoulder moves and lead to long-term problems if not fixed.
Shoulder surgeons also consider how large the broken pieces are, where they’re located, and how the ball of the shoulder joint (the humeral head) is sitting in the socket. The goal of surgery is to put the joint surface back in the right position so your shoulder can move smoothly again.
Carefully choosing the right time and method for surgery plays a big role in how well your shoulder works after recovery.
Minimally Invasive Surgery: Arthroscopic Repair of Glenoid Fractures
Thanks to advances in medical technology, many glenoid fractures can now be treated using arthroscopic techniques—a minimally invasive type of surgery. Instead of making a large incision, the surgeon uses small tools and a camera inserted through tiny cuts to repair the damaged area. This approach usually means less pain after surgery, faster healing, and a lower risk of complications.
The type of arthroscopic procedure used depends on the kind of fracture. For example, small fractures along the front edge of the socket (called anterior rim fractures) can often be repaired entirely through the scope. During this procedure, the surgeon cleans out any scar tissue or blood clots and carefully repositions the broken bone.
In more complex cases, like large fractures inside the socket (known as glenoid fossa fractures), surgeons may combine arthroscopy with more traditional methods to secure the bone fragments with screws or other hardware. This blended approach helps ensure the joint is stable and heals correctly.
Postoperative Care and Rehabilitation
Postoperative care and rehabilitation are critical components of the recovery process following surgical treatment of glenoid fractures. Initially, patients undergo a period of immobilization to facilitate initial healing, followed by the commencement of passive range-of-motion exercises. These exercises are crucial in preventing stiffness and maintaining some degree of mobility in the shoulder.
Around six weeks post-injury, strengthening exercises are introduced to rebuild muscle strength and support around the shoulder. The progression from passive to more active engagement in exercises is carefully monitored to ensure the shoulder heals correctly. The rehabilitation timeline can vary, often extending up to one year for full functional recovery.
Rehabilitation aims to restore normal shoulder mobility and strength, enabling patients to resume daily activities without pain or limitations. Achieving this requires diligence and adherence to the prescribed rehabilitation regimen.
What to Expect After a Glenoid Fracture
The good news is that most people recover well from glenoid fractures—whether treated with or without surgery. With the right care and commitment to physical therapy, many patients regain strong, functional shoulders and return to their regular activities.
If you have surgery, following your rehab plan closely and keeping up with your follow-up appointments is key to a smooth recovery. Your doctor will use X-rays or other imaging to check how your shoulder is healing over time.
The final outcome depends on a few things, like how serious the fracture was, how the surgery was done (if needed), and how well you stick to the rehabilitation process. Most patients who stay on track with their recovery plan see great results.
Summary
Glenoid fractures are uncommon but important injuries that affect the socket part of your shoulder joint. They can be difficult to treat, so seeing an experienced shoulder surgeon is important.
In some cases, surgery—especially using minimally invasive techniques like arthroscopy—is the best way to repair the damage and restore shoulder movement. After surgery or other treatment, physical therapy and regular check-ins with your doctor are key parts of a successful recovery.
The outlook for people with glenoid fractures is encouraging, and with ongoing research and new technology, treatments are getting better all the time. Staying informed and following your care plan can make a big difference in your recovery and long-term shoulder health.
Frequently Asked Questions
What is a glenoid fracture?
A glenoid fracture refers to a break in the glenoid, the socket in the shoulder blade that accommodates the head of the upper arm bone. This type of injury can significantly impact shoulder stability and function.
How are glenoid fractures diagnosed?
Glenoid fractures are diagnosed primarily through imaging techniques such as X-rays and CT scans, complemented by a thorough physical examination. This approach ensures an accurate assessment of the injury.
When is surgery needed for a glenoid fracture?
Surgery is required for glenoid fractures with significant displacement, instability, or when a large portion of the intra-articular surface is affected. These conditions ensure proper function and alignment of the shoulder joint post-injury.
What are the potential complications of glenoid fracture surgery?
Complications of glenoid fracture surgery may include infection, nerve injury, shoulder stiffness, and potential damage to the cartilage, which increases the risk of arthritis. It’s essential to discuss these risks with your healthcare provider for informed decision-making.
What does postoperative care for glenoid fracture surgery involve?
Postoperative care for glenoid fracture surgery includes initial immobilization, followed by a structured regimen of passive and active range-of-motion exercises to promote shoulder mobility and strength recovery. This approach is essential for optimal healing and regaining function.





