Are you worried that the discomfort and limited movement in your shoulder might be arthritis? Recognizing “what are the signs of arthritis in the shoulder” early on, such as persistent pain, stiffness, or limited motion, can be crucial in managing the condition.
This post will provide you with the essential markers and considerations for shoulder arthritis, guiding you towards understanding your symptoms and next steps.
Key Takeaways
- Shoulder arthritis symptoms include persistent pain, stiffness, limited range of motion, weakness, and a grinding or clicking sensation in the joint, which, if left untreated, could lead to a progressive loss of function.
- Arthritis affects various parts of the shoulder anatomy, including the glenohumeral and AC joints, causing compromised stability, increased friction, and destruction of cartilage; imaging tests help reveal the severity of these impacts.
- Treatment for shoulder arthritis ranges from nonsurgical options like medication and physical therapy to surgical interventions such as shoulder replacement surgery, followed by a critical post-surgery care and rehabilitation phase.
Decoding the Discomfort: Identifying Symptoms of Shoulder Arthritis
When shoulder arthritis creeps in, it’s more than just a nuisance; it’s a signal from your body that something is amiss within the intricate structures of your shoulder joint. If these shoulder arthritis symptoms are ignored, it could lead to a progressive loss of function. Hence, early recognition and treatment are vital to maintain an active lifestyle. Whether you’ve noticed persistent pain or an inexplicable loss of strength, understanding these symptoms is your first line of defense against the progression of this condition. Some common symptoms of shoulder arthritis include:
- Persistent pain in the shoulder joint
- Stiffness and limited range of motion
- Weakness in the shoulder muscles
- Swelling and inflammation
- Grinding or clicking sensation in the shoulder joint
If you experience any of these symptoms, it is important to consult with an orthopedic surgeon who specializes in shoulders for an accurate diagnosis and appropriate treatment.
Here are some common signs that indicate it’s time to take action.
Persistent Shoulder Pain as a Common Symptom
The constant companion of shoulder arthritis is shoulder arthritis pain, a deep-seated ache that seems to emanate from within the joint itself. It can be as capricious as the weather, sometimes intensifying with rain or cold, leaving you longing for relief. This isn’t a pain that fades after a day’s rest; it can be so relentless that even the simplest movements, such as:
- reaching for a high shelf
- lifting objects
- putting on clothes
- combing your hair
become daunting tasks.
Planning your day to avoid certain arm movements indicates that your shoulder pain is not merely temporary discomfort. It suggests a deeper issue within the glenohumeral shoulder joint.
Swelling and Tenderness in the Shoulder Joint
Swelling and tenderness are the silent alarms of shoulder arthritis, red flags that should not be ignored. Inflammation within the joint space can manifest as a subtle puffiness around the shoulder blade or as a more pronounced swelling that makes your joint feel warm to the touch. The pain often peaks at the top of your shoulder, especially with acromioclavicular (AC) joint arthritis, signaling an urgent cry for attention from your body.
More pronounced redness and warmth, especially in rheumatoid arthritis cases, clearly indicate an internal struggle in your shoulder against the very tissues designed to protect it.
Loss of Range of Motion and Stiffness
The freedom to move our arms in all directions is something we often take for granted—until arthritis begins to erode that liberty. A stiffening shoulder joint can quietly steal away your range of motion, hindering even basic self-care activities like showering or getting dressed. The once wide arc of movement becomes smaller and smaller, as if your arm is being held back by an unseen force.
Loss of mobility isn’t just inconvenient. It signifies degenerative changes within your joint, a silent progression that can significantly impact your quality of life if not addressed.
The Anatomy of Arthritis: How Shoulder Joints are Affected
Understanding arthritis of the shoulder requires a look beneath the skin, to where the complex dance of bones, cartilage, and soft tissues occurs. The shoulder is not just a single joint but a symphony of structures working in harmony to afford you the mobility you rely upon daily. When shoulder arthritis enters the picture, it disrupts this harmony, leading to compromised stability, increased friction, and the gradual destruction of the very elements that facilitate your shoulder’s movement.
From the glenohumeral joint to the AC joint, arthritis spares no part, leaving its mark on bones and soft tissues alike. Here’s how this condition impacts different parts of your shoulder’s anatomy.
Understanding the Glenohumeral Joint’s Role
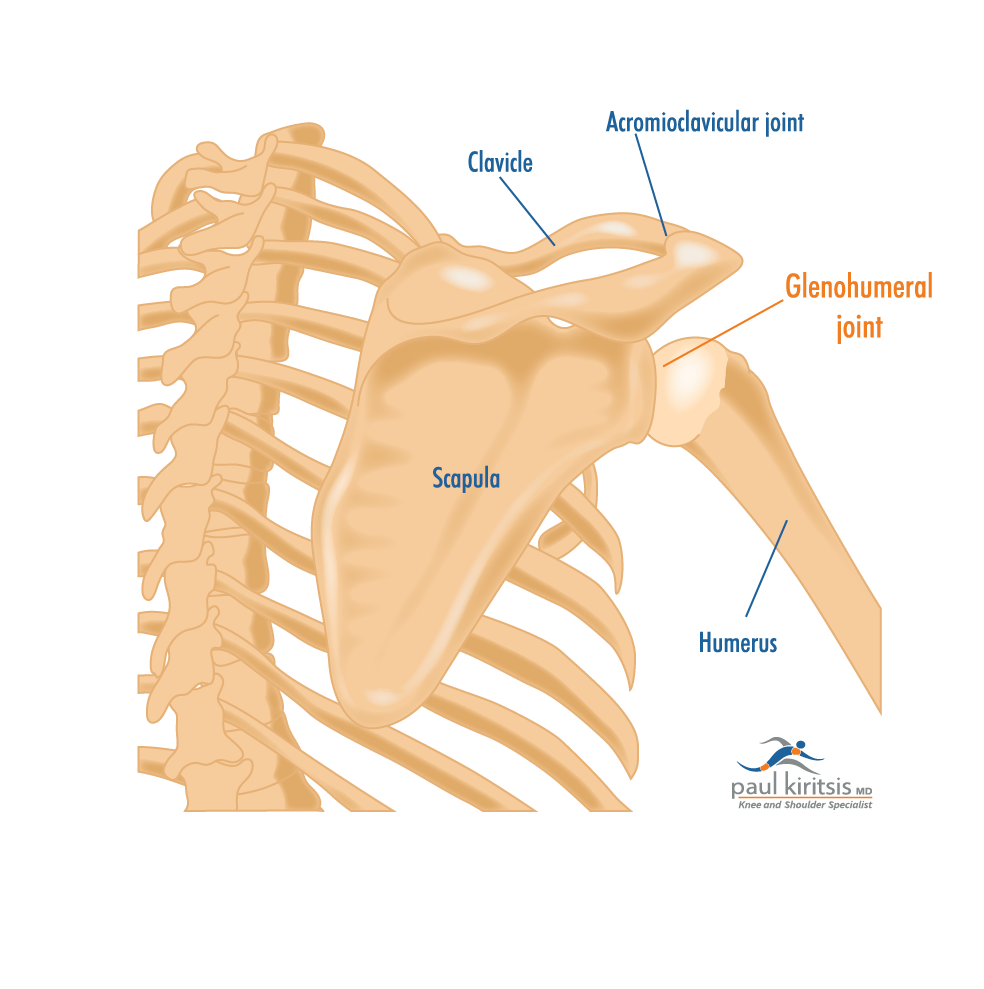
The glenohumeral joint, a pivotal player in your shoulder’s mobility, is often the first to suffer under the weight of arthritis. This ball-and-socket joint, where the humerus meets the scapula, relies on a smooth cartilage surface to facilitate movement—a surface that erodes with the onset of arthritis.
Pain localized at the side of the shoulder is a telltale sign of trouble brewing in the glenohumeral joint, distinct from the discomfort associated with AC joint arthritis, which typically occurs at the shoulder’s top. As this cartilage wears away, bone grinds against bone, sparking pain and limiting your shoulder’s once-fluid motion.
The Impact on the AC Joint and Surrounding Soft Tissues
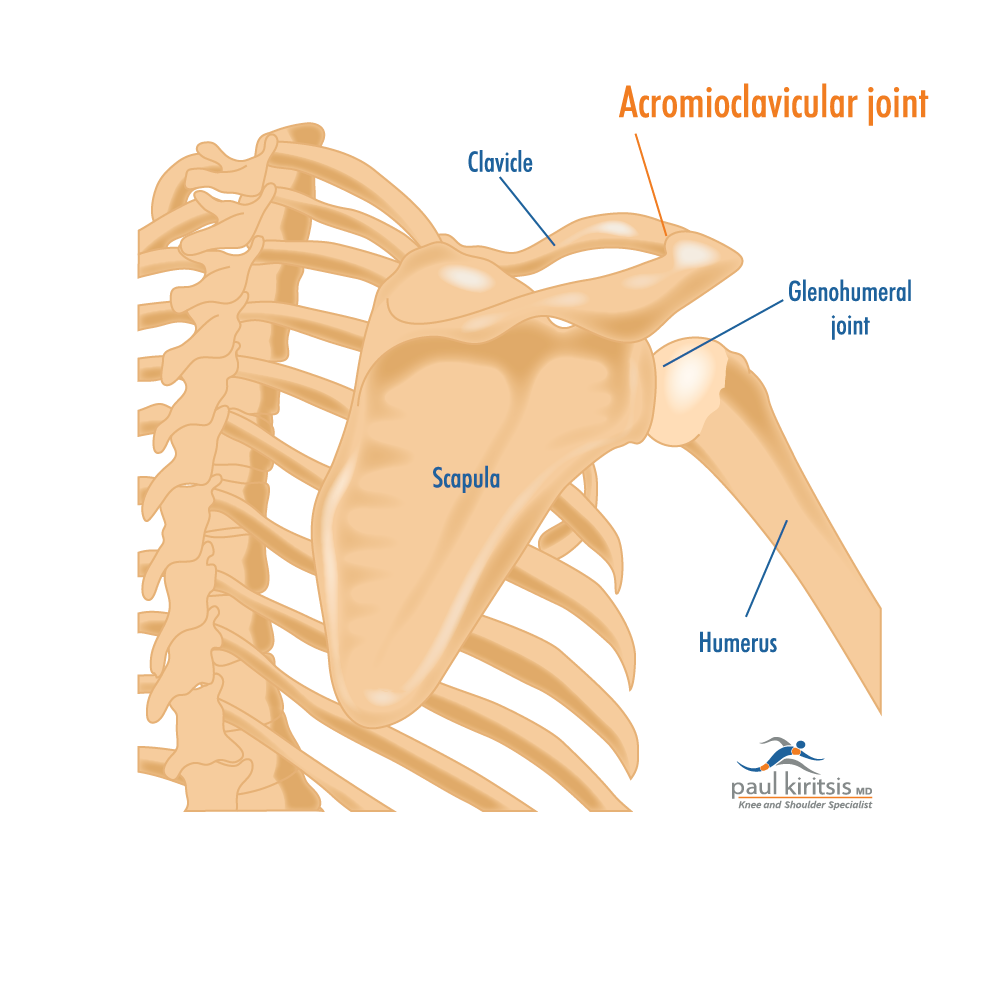
Equally important is the AC joint, a bridge connecting your shoulder blade to your collarbone, as well as the upper arm bone. It’s here that arthritis can cause a narrowing of the joint space, leading to the formation of bone spurs and a loss of the smooth articulation that once characterized your shoulder movements. An X-ray can reveal the extent of arthritis in the AC joint, sometimes suggesting a risk for rotator cuff injury—a scenario that underscores the interconnectedness of the shoulder’s anatomy.
The surrounding bursae and soft tissues also feel the impact, as their role in reducing friction and supporting smooth movement becomes compromised by arthritis. Pain in the AC joint’s anterior-superior location is a diagnostic clue that brings into focus the multifaceted nature of shoulder arthritis.
Differentiating Types of Shoulder Arthritis
Not all shoulder arthritis is created equal. The term “arthritis” may be a catch-all, but within its grasp are distinct types, each with its own set of causes and symptoms. Some common types of shoulder arthritis include:
- Osteoarthritis: caused by wear-and-tear on the joint
- Rheumatoid arthritis: an autoimmune condition where the immune system attacks the joint
- Post-traumatic arthritis: occurs after an injury to the shoulder joint
Understanding these differences is crucial for effective management.
Each form of arthritis carries its unique challenge, whether it’s the gradual breakdown of cartilage or the inflammatory onslaught against joint linings. We’ll dissect the unique characteristics of each type.
Osteoarthritis: The Wear-and-Tear Challenge
Osteoarthritis of the shoulder is likened to a tire that’s worn down over time. The cartilage that once allowed for smooth movement begins to fray and deteriorate, leading to the exposure of underlying bone and the painful reality of a joint in distress. It’s a condition that doesn’t happen overnight; it follows a gradual course, from the softening of cartilage to the formation of deep fissures and, ultimately, the complete erosion of this cushioning layer.
For those grappling with osteoarthritis, the wear-and-tear challenge is a daily struggle against stiffness and pain that worsens with each passing year.
Rheumatoid Arthritis: An Autoimmune Battle
Rheumatoid arthritis, on the other hand, is an internal battle, where the immune system, confused and misguided, turns against the body’s own joint linings. It’s a form of inflammatory arthritis that can cause the shoulder joint to swell, and ache, often affecting both shoulders simultaneously—a hallmark distinction from other types.
The disease’s progression is marked by the erosion of cartilage and the painful bone-on-bone contact that results from such destruction. Those living with rheumatoid arthritis may hear their shoulders crackle with movement, a grim reminder of the damaged cartilage surfaces that lie beneath.
Post Traumatic Arthritis: Aftermath of Injury
Trauma to the shoulder, such as a fracture or dislocation, can set the stage for post-traumatic arthritis, a condition that lurks in the shadows of past injuries. Unlike osteoarthritis, which emerges from the natural wear of time, post-traumatic arthritis is born from the damage inflicted by a specific event—leaving behind scar tissue and an altered joint surface that can lead to pain and stiffness.
The burden of this arthritis type lies not only in the immediate aftermath of injury but in the long-term effects that can significantly hinder one’s ability to engage in everyday activities due to:
- limited mobility
- chronic pain
- joint stiffness
- decreased range of motion
When to Seek Medical Advice: Diagnosing Shoulder Arthritis
Navigating the waters of shoulder arthritis is not a journey to undertake alone. Knowing when to seek medical advice is a crucial step in diagnosing and managing the condition. The diagnostic process is multifaceted, combining patient medical history, a nuanced physical exam, and advanced imaging tests to paint a comprehensive picture of the shoulder’s health.
We’ll examine how we as orthopedic surgeons decipher the complexities of shoulder arthritis to determine the most effective course of action.
The Role of Medical History in Diagnosis
Your medical history is akin to a detective’s case file, providing valuable clues that contribute to an accurate diagnosis of shoulder arthritis. A thorough history accounts for factors such as age, occupational hazards, and previous injuries, all of which can influence the presentation and progression of the condition.
The onset of pain, the triggers that aggravate it, and the effectiveness of past treatments—all these pieces come together to form a narrative that guides the diagnostic process. A well-documented medical history can even reduce the need for further diagnostic tests, highlighting the importance of a comprehensive patient interview.
Physical Examination Insights
A physical examination serves as the hands-on chapter of the diagnostic story. Through visual inspection and palpation, doctors can assess swelling, muscle weakness, and changes in joint appearance that may indicate osteoarthritis. Gentle pressure applied during the exam can help localize pain and discomfort, offering insights into the joint’s condition.
These findings, coupled with the patient’s reported symptoms, help to form a clearer picture of the underlying issue—be it a rotator cuff tear involving the rotator cuff tendons or the hallmark signs of degenerative joint disease.
Imaging Tests: Revealing the Inner Workings
Imaging tests are the windows into the internal workings of the shoulder joint, revealing what the eye cannot see. Here are the different types of imaging tests that can be used:
- X-rays: X-rays show bone changes and joint space narrowing that are synonymous with arthritis.
- MRI scans: MRI scans provide a detailed view of soft tissues and bone.
- CT scans: CT scans offer cross-sectional images that can highlight bony defects and assist in surgical planning.
These tests are not just about confirming the presence of arthritis; they are about understanding its severity and laying the foundation for a targeted treatment plan.
Addressing Arthritis: Treatment Options for Shoulder Pain Relief
The quest for pain relief from shoulder arthritis is not a one-size-fits-all endeavor. Treatment options range from simple lifestyle adjustments and nonsurgical methods to more invasive surgical solutions. Each patient’s experience with arthritis is unique, and so too should be their treatment plan.
Whether it’s managing symptoms through medication and physical therapy or considering shoulder replacement surgery, the goal is to alleviate pain and restore function. We’ll discuss different options available for those seeking relief from arthritis pain.
Nonsurgical Treatments: First Line of Defense
Before the thought of surgery enters the picture, there are numerous nonsurgical treatments that can serve as the first line of defense to treat arthritis, particularly shoulder arthritis. These conservative measures focus on managing pain, maintaining range of motion, and modifying activities to avoid exacerbating symptoms. Medications like acetaminophen or NSAIDs, along with hot or cold therapy, can offer temporary relief from the aches of arthritis. Injections, such as cortisone or hyaluronic acid, may provide more lasting pain relief, though they come with their own set of considerations.
For many, these nonsurgical treatments can be a lifeline, providing the respite needed to continue with daily activities.
Surgical Solutions: Considering Shoulder Replacement Surgery
However, when nonsurgical methods fail to keep the pain at bay, surgical solutions come into play. Shoulder replacement surgery, including Precision Shoulder Replacement is tailored to the individual’s condition, and can offer great hope for those with advanced arthritis. This operation, whether it be an anatomic total shoulder replacement or a reverse total shoulder replacement, aims to restore joint function and provide long-term pain relief.
For patients with lower grades of arthritis, arthroscopic shoulder debridement might serve as a less invasive option, offering temporary respite from discomfort. Surgical intervention is a significant decision, one made with careful consideration of the patient’s specific needs and the potential for improved quality of life post-procedure.
Embracing Recovery: Post-Surgery Care and Rehabilitation
The conclusion of shoulder surgery marks the beginning of a new chapter: the journey toward recovery. Post-surgery care and rehabilitation are critical to ensuring the success of the procedure and the patient’s return to normalcy. This period is characterized by efforts to minimize inflammation, manage post-operative pain, and protect the integrity of the surgical repair. Collaborative communication between the surgical and rehabilitation teams is paramount, aligning treatment goals and methodologies for the best outcome.
We’ll examine the stages of physical therapy and home care practices that promote a smooth and efficient recovery process.
The Journey Through Physical Therapy
Physical therapy is the cornerstone of recovery after shoulder joint replacement, guiding patients through a carefully structured program designed to reduce pain and regain function. The therapeutic process begins with gentle exercises to promote range of motion, gradually transitioning to more active strengthening routines. Each step of the way, therapists assess the patient’s progress, tailoring the program to ensure optimal healing while minimizing strain on the repaired tissues.
Through a combination of exercises, stretches, and massages, patients reacquaint themselves with the full capabilities of their shoulders, setting the stage for a return to the activities they love.
Home Care and Lifestyle Adjustments Post-Surgery
Once home, the recovery process continues with practical adjustments to daily living. Keeping the surgical site clean and dry is paramount, using waterproof bandages to protect the incision during showers. Dietary changes, such as incorporating high-fiber foods and staying hydrated, help circumvent constipation, a common side effect of post-surgical medication.
Simple modifications to clothing and bathing tools can make self-care manageable, while arranging for transportation and assistance with household chores ensures a safe and stress-free environment. Emotional well-being is equally important, and maintaining social connections can provide a much-needed morale boost during the healing period.
Summary
In the quest to conquer shoulder arthritis, knowledge is power. Recognizing the symptoms early, understanding the anatomy of the shoulder, distinguishing between types of arthritis, and exploring treatment options are all critical steps in managing this condition. Whether through nonsurgical methods, advanced surgical techniques like Precision Shoulder Replacement, there are paths to pain relief and restored mobility. By embracing the recovery process with diligence and care, patients can have the opportunity to reclaim the freedom of movement that shoulder arthritis once threatened to take away.
Frequently Asked Questions
What is the end stage of arthritis in the shoulder?
The end stage of arthritis in the shoulder is characterized by the progressive wear down of cartilage, causing the bones to painfully rub against each other during movement, resulting in severe pain and loss of function. This is often visible on X-rays as bone-on-bone contact and the development of bone spurs.
How do I know if I have arthritis in my shoulder?
If you are experiencing pain in the shoulder joint, stiffness, and reduced range of motion, these could be symptoms of shoulder arthritis. Consider nonoperative treatments such as stretches, lifestyle modifications, applying ice or heat, and taking medication to manage the pain.
What are the most common symptoms of shoulder arthritis?
The most common symptoms of shoulder arthritis are persistent pain, swelling, tenderness, and stiffness, which can result in a reduced range of motion in the joint.




